
Eosinophilic Gastrointestinal Disorders Program
The Eosinophilic Gastrointestinal Disorder Program at Children’s Hospital Los Angeles provides comprehensive and specialized care for infants, children and teens living with Eosinophilic Esophagitis (EoE) and other Eosinophilic Gastrointestinal Disorders (EGID). Experts from different specialties come together to perform a thorough evaluation and develop a treatment plan tailored to your unique needs.
What are eosinophils?
Eosinophils are a type of blood cell that are a normal part of the immune system. They help us fight certain types of infections such as parasites. When activated by environmental or food triggers, eosinophils can cause allergic inflammation. Their active state is called “degranulating.”
What are EGID and EoE?
EGID is a group of disorders resulting from an abnormal build-up of eosinophils in the gastrointestinal (GI) tract leading to ongoing inflammation and discomfort. EoE is the most common form of EGID and primarily affects the esophagus.
People with EGID may experience abdominal pain, diarrhea, weight loss, slow growth and mealtime difficulties. People with EoE may experience difficulty swallowing, repeated vomiting, acid reflux symptoms, and food impaction (when food gets stuck in the food pipe or esophagus).
To diagnose EGID we use a combination of laboratory tests, imaging and procedures including endoscopy.
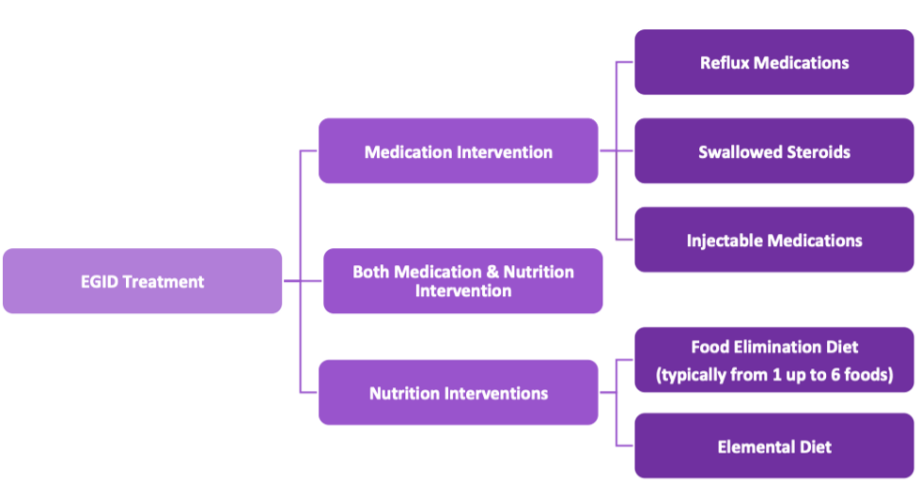
Treatment may include medications, dietary changes, or a combination of both. Each patient is unique, and we work with you to personalize your treatment plan.
We treat these conditions:
- Eosinophilic Esophagitis (EoE: affecting the esophagus)
- Eosinophilic Gastritis (EG: affecting the stomach)
- Eosinophilic Gastroenteritis (EGE: affecting the stomach and small intestine)
- Eosinophilic Enteritis (EE: affecting the small intestine)
- Eosinophilic Colitis (EC: affecting the large intestine)
Diagnosis of EGID requires endoscopy
Currently, EGID can only be diagnosed by a procedure called endoscopy. Endoscopy uses a camera to visualize the inside of the gastrointestinal (GI) tract and obtain small tissue samples that are examined under a microscope to look for eosinophils. Often, repeated endoscopies are required to evaluate your response to treatment.
Transnasal Endoscopy is an option
At Children’s Hospital Los Angeles, we proudly offer Transnasal Endoscopy (TNE) as an alternative to traditional endoscopy for suitable candidates. We are one of the few EGID programs in the U.S. to offer this procedure. TNE is performed without sedation and offers a way to examine the GI tract without repeated exposures to general anesthesia. For more information, visit the CHLA TNE Program (https://www.chla.org/transnasal-endoscopy-program).
We may recommend other diagnostic tests including:
- Blood tests to measure blood levels of eosinophils
- Allergy testing by skin tests and/or blood levels of allergic antibody (IgE) to triggers
- Stool tests to look for chronic inflammation
- Specialized imaging studies including X-rays to examine the esophagus (food pipe)
We can treat EGID with medications and specialized diets
The type of treatment we recommend varies based on the location of the inflammation, its severity, and your preferences. Treatment options may include medications that reduce inflammation, customized food elimination diets, or a combination of both. See detailed descriptions below.
We work closely with patients and families to determine the best options, whether it is medication and/or dietary changes.
We can use a number of medications to treat EGID
Proton pump inhibitor (PPI)
PPIs are medications that reduce the production of stomach acid. They are effective treatment of EoE in likely one of 2 ways: 1. they treat acid reflux that can make EoE worse. 2. PPIs also target the allergic inflammatory pathway involved in EoE. This is commonly referred to as ‘PPI-responsive EoE.’
Swallowed (topical) steroids
Steroids are very effective in controlling allergic inflammation. Inhaled steroids are widely used in treating asthma. We use them in a different way to treat EoE. When these preparations are taken by mouth daily, they coat the surface of the esophagus to calm the inflammation resulting from EoE, reducing reactions to EoE triggers. These medications are minimally absorbed and unlikely to cause undesired steroid side effects.
Commonly used topical steroid preparations are:
- Fluticasone
An inhaler you spray directly into your mouth and swallow - Budesonide slurry
A small liquid packet you mix with honey, syrup, Splenda, or apple sauce into a thick liquid consistency and swallow to coat the esophagus
After taking a swallowed steroid, it is important that you do not eat or drink for at least 30 minutes
Systemic steroids
Oral systemic steroids may be used to provide more immediate control of inflammation. Prednisone and Prednisolone are absorbed by the body rapidly and are very effective in calming inflammation. However, they also have more side effects and long-term use requires careful monitoring. Budesonide capsule is another oral steroid that is less absorbed and therefore associated with less side effects but can still be effective in treating inflammation in the lower GI tract. Prednisone, Prednisolone, and Budesonide have been used to treat eosinophilic gastritis, enteritis, colitis, or EoE refractory to conventional treatments.
Injectable Medications (Biologics)
These medications target specific molecules involved in the inflammatory pathway that leads to EGID. Currently, Dupixent (Dupilumab) is the only Food and Drug Administration (FDA)-approved medication for adults and older children with EoE.
Dupixent (Dupilumab)
Dupixent has been widely used in adults and children with severe eczema and asthma with great success and an excellent safety profile. On May 20, 2022 Dupixent was approved by the Food and Drug Administration (FDA) for treating EoE in selected patients, making it the first FDA-approved medication for EoE. This is an injectable medication you learn to give at home that offers another “steroid-free” option.
There are several other biologic medications that are actively being developed to treat EGID. Some patients may receive these medications as research participants in clinical trials.
Meet Our Team
We offer state of the art care in a supportive environment to help people and their families living with EGID and EoE. We provide multidisciplinary care with a team of experts from multiple specialties that work together to address the full scope and impact of these conditions. We work with you to develop a comprehensive and personalized treatment plan that best fits with you and your family’s unique needs and challenges.
The multidisciplinary EGID team includes:
- Allergy Doctor, Board-certified pediatric allergist with expertise in EGID
- GI Doctor, Board-certified pediatric gastroenterologist with expertise in EGID
- Therapist, PhD. Psychologist with expertise in EGID and food allergy to support you throughout diagnosis, treatment and lifestyle changes
- Registered Dietitian/Nutritionist with expertise in EGID and other forms of food allergy to optimize nourishment and satisfaction on a restricted diet
- Registered Nurse as clinic coordinator to support you and your individualized care plans
- Referral as needed to Occupational and Speech Therapists who specialize in feeding difficulties
Affiliated Providers
Jennifer Hershfield, PhD (Pediatric Psychology)
Jill Madison (Registered Dietician)
Niaz Lavee (EGID RN Coordinator)
Clinical Trials and Research
As a means of ensuring continuing excellence and state of the art patient care, the Eosinophilic Gastrointestinal Diseases Program at CHLA conducts prospective outcomes research. This is important in making improvements in care to patients seen in our program and other programs. Patients evaluated in our clinic may be consented for participation in this research. Patient information is always protected and confidential and the study is approved by the CHLA Institutional Review Board.
Food Elimination
Dietary changes, or nutrition interventions, are an effective treatment for EoE and EGID. There are several stepwise approaches ranging from avoiding one or more food groups, to the most significant and restrictive nutrition intervention, which is an elemental formula-only diet.
When deciding if an elimination diet works for your family, there are several considerations. To help guide your decision, you will meet with a RD (Registered Dietitian) who specializes in organizing food and designing plans to meet the nutritional needs for your child. The RD can provide strategies to identify safe foods, recognize hidden ingredients, and determine appropriate food substitutes to maintain a balanced and nutritionally appropriate diet for ongoing optimal growth.
Additional factors to consider in discussing elimination diets include:
- Your child’s feeding development, growth, preferences, and age
- Ability to read food labels and safe alternates
- Family commitment and/or household dynamics
- Expense
Typically, a food group or groups is eliminated for a minimum of 8-12 weeks before re-scoping to assess the effect of this dietary change. Unfortunately, allergy testing (both skin and/or blood tests) cannot predict which foods should be eliminated. Endoscopic evaluation is the best way to know if a dietary change promotes healing.
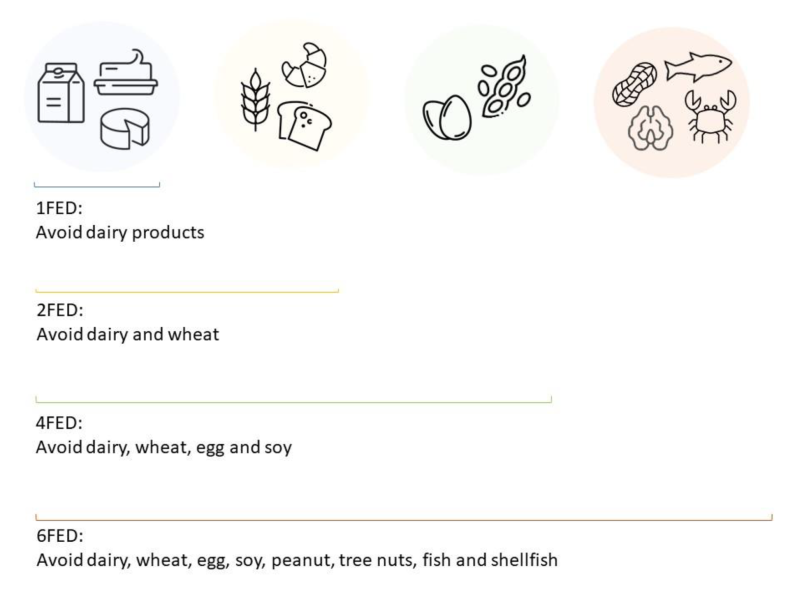
Elimination diet categories are detailed below, you’ll note increasing levels of dietary restriction have greater levels of successfully inducing remission or healing.
- One Food Elimination Diet (1FED): The “one” food eliminated refers to removing all dairy products, including any form of dairy (cow, goat, sheep or any mammal), whether dry, liquid, condensed milk, cheese, yogurt and butter. Dairy has been found to be the most common trigger food for eosinophilic disease, EGID. Whether milk is positively identified on a skin, blood, or oral challenge, the avoidance of dairy products remains useful and a valid first line choice. Elimination of dairy products alone is associated with healing in 33-65% of children with EoE.
- Two Food Elimination Diet (2FED): This intervention removes dairy (as described above) and all wheat products. These are the two most common food allergen triggers for EGID. Wheat products include anything made with wheat flour such as bread, pasta, and baked goods. Learning to read food labels and find substitute foods is required as wheat is commonly found in processed foods. While many substitutes for milk and wheat are available, finding appetizing options in different settings can be a challenge. Nearly half of children with EoE respond favorably to 2FED.
- Four Food Elimination Diet (4FED): This intervention continues with the elimination of both milk and wheat as above, with the addition of the next two most likely triggers for EoE/EGID, which are egg and soy. In total, these 4 ingredients are quite pervasive in processed foods. Nutritional counseling is essential to avoid these potential triggers and find suitable substitutes to maintain nourishment and enthusiasm for eating. Over half of children with EoE have a healing response to 4FED.
- Six Food Elimination Diet (SFED or 6FED): This is the most well-studied and effective of form of food elimination diet in EoE and EGID. This intervention removes the top 8 food allergens: milk, wheat, egg, soy, peanut/tree-nut, fish/shellfish with success rates for inducing remission consistently greater than 70%. Typically, after remission is achieved with 6FED and confirmed by endoscopy, individual food groups are reintroduced one at a time. This is followed by repeat endoscopy in 8-12 weeks to monitor disease with the goal of identifying culprit foods and removing them permanently while allowing safe foods back into diet. Classically, each reintroduction is followed by endoscopy with biopsy. However, reintroduction methods are evolving based on desired scope frequency and clinical remission. While 6FED may sound daunting, remember that these foods are common allergens in the US, thus the FDA mandates the use of plain language in the ingredients list of food packages to identify these allergens.
- Elemental diet, or Total Elimination Diet (ED): This intervention removes all food and replaces food intake with an elemental, amino acid-based hypoallergenic formula. This approach is the strictest as well as the most effective, with the highest consistent efficacy rate for both EoE and EGID. Success rates for EoE are as high as 90-95%. However, adherence is difficult as eating is interrupted. The potential benefit must be balanced with the social, psychological, and developmental impact of regular food intake. Considerations for selecting this restrictive, yet very effective elimination diet, include social, developmental, nutritional, and financial (depending on insurance benefit coverage) challenges.
Food Diary
Resources
- North American Society for Pediatric Gastroenterology, Hepatology and Nutrition
- American Partnership for Eosinophilic Disorders: What are EGIDs?
- American Partnership for Eosinophilic Disorders
- CURED: Campaign Urging Research for Eosinophilic Disease
- GIKids: Eosinophilic Esophagitis
- American Academy of Allergy, Asthma & Immunology: Eosinophilic Esophagitis


