Children’s Hospital Los Angeles Receives NIH Awards for Research Into Combating Childhood Kidney Failure
LOS ANGELES (November 2, 2022) — In children with progressive chronic kidney disease (CKD), loss of kidney function is mostly irreversible. The GOFARR Laboratory for Organ Regenerative Research and Cell Therapeutics in Urology at Children’s Hospital Los Angeles has received an award from the National Institutes of Health (NIH) to conduct research into the underlying biological mechanisms that cause kidney failure and to develop new treatments to protect kidney function. Laura Perin, PhD, who co-directs the GOFARR Laboratory, and Stefano Da Sacco, PhD, are co-Principal Investigators on the five-year $3.2 million grant focused on Alport syndrome, a type of CKD.
Dr. Perin is the Principal Investigator on another NIH grant, part of a two-year $2 million award shared with collaborators, for the second phase of developing an innovative kidney-on-a-chip platform to test medications for chronic kidney disease.
Preserving kids' podocytes
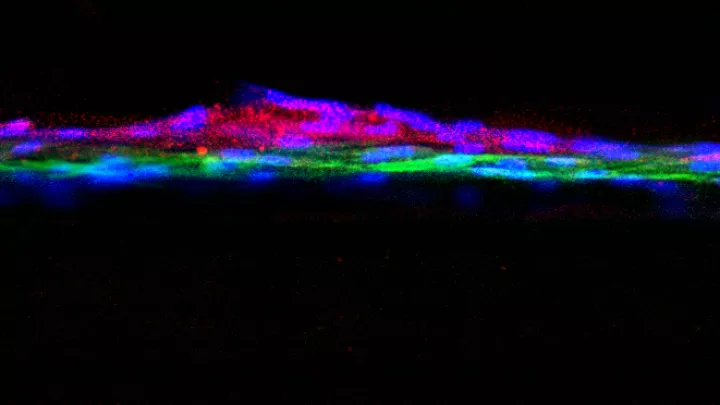
Chronic kidney disease progressively destroys a highly specialized kidney structure: the glomerulus, which filters blood.
“The glomerulus is where the kidney filters the blood,” says Dr. Perin. "When the glomeruli are not functioning, our kidneys are destined to fail. Patients’ only options are dialysis or transplantation as there is no direct therapy for preserving the glomerulus structure. Our patients with chronic kidney disease take medications for lowering blood pressure, but they have no medications to specifically prevent degeneration of the glomerulus.”
As a result, the glomerulus irretrievably loses its working podocytes, the specialized cells that filter waste and maintain the body’s fluid balance. “When you lose enough podocytes, over time your kidneys will not filter anymore," says Dr. Perin, who is also an Associate Professor at the Keck School of Medicine of USC. “These podocytes are among the few types of cells in our body with a very scarce probability of regeneration. When the podocytes lose their function, they die and are lost in the urine.”
The NIH awards will support the GOFARR Lab’s investigations into the causes of kidney failure in CKD. According to Dr. Perin, gaining insight into the pathways responsible for podocyte damage could guide the discovery of new therapeutics to potentially slow or even reverse CKD progression.
GOFARR researchers are studying the effects of microRNA—a very small RNA that can be used to control protein expression in cells. The researchers will examine how controlling levels of a specific mRNA, miR-193a, could “re-program” the molecular signaling networks that influence how podocytes function. Learning how to manipulate the interactions between these cells could help develop a therapy to protect podocytes.
“This will be one of the first kinds of therapies designed to just work within the glomeruli,” says Dr. Perin. “We are targeting one specific cell type in this model of Alport syndrome that is the culprit of this disease. We have actually found something that we can therapeutically target that can possibly affect patients with kidney disease.”
3D kidney-on-a-chip
So far, developing medications that can directly target the underlying causes of chronic kidney disease has been hampered by the lack of reproducible in-vitro models. The GOFARR Lab’s second NIH award will enable the further development of the kidney-on-a-chip platform to screen biomarkers that could lead to potential therapies. This hybrid tool created by GOFARR researchers and their partners features a chip with surface compartments loaded with living kidney cells that serve as a glomerular filtration barrier for testing medications in the laboratory. “We recreated the glomerulus on a chip for drug screening,” comments Dr. Perin.
GOFARR researchers and their collaborators are scaling up the kidney-on-a-chip for use by the scientific community and pharmaceutical companies to conduct drug screening and testing, as well as for building models of glomerular filtration barrier dysfunction to mimic other chronic kidney diseases.
“We are studying three or four different types of chronic kidney diseases under an NIH-sponsored project,” says Dr. Perin. “The more you study a disease from different angles, the more you can understand the disease.”
About Children’s Hospital Los Angeles
Children’s Hospital Los Angeles is at the forefront of pediatric medicine, offering acclaimed care to children from across the world, the country and the greater Southern California region. Founded in 1901, Children’s Hospital Los Angeles is the largest provider of care for children in Los Angeles County, the No. 1 pediatric hospital in the Pacific region and California, and among the top 10 in the nation on U.S. News & World Report’s Honor Roll of Best Children’s Hospitals. Clinical expertise spans the pediatric care continuum for newborns to young adults, from everyday preventive medicine to the most advanced cases. Inclusive, kid- and family-friendly clinical care is led by physicians who are faculty members of the Keck School of Medicine of USC, and proven discoveries reach patients faster through The Saban Research Institute of Children’s Hospital Los Angeles—among the top 10 children’s hospitals for National Institutes of Health funding. The hospital also is home to the largest pediatric residency training program at a freestanding children’s hospital in the western United States. To learn more, follow us on Facebook, Instagram, LinkedIn, YouTube and Twitter, and visit our blog at CHLA.org/blog.