Spill Your Guts: Pediatric Gastroenterologist Talks Fecal Transplants
Bloating, gas, abdominal pain and diarrhea are physically uncomfortable and often taboo topics, but for children with gastrointestinal (GI) disorders, these symptoms dictate day-to-day life.
With two clinical trials exploring the efficacy of fecal—yes, fecal—transplants in kids with GI disorders, we asked Sonia Michail, MD, CPE, AGAF, FAAP, a pediatric gastroenterologist and nutritionist at Children’s Hospital Los Angeles (CHLA) to explain her work.
We’ve recently been hearing a lot about the microbiome, but what is it?
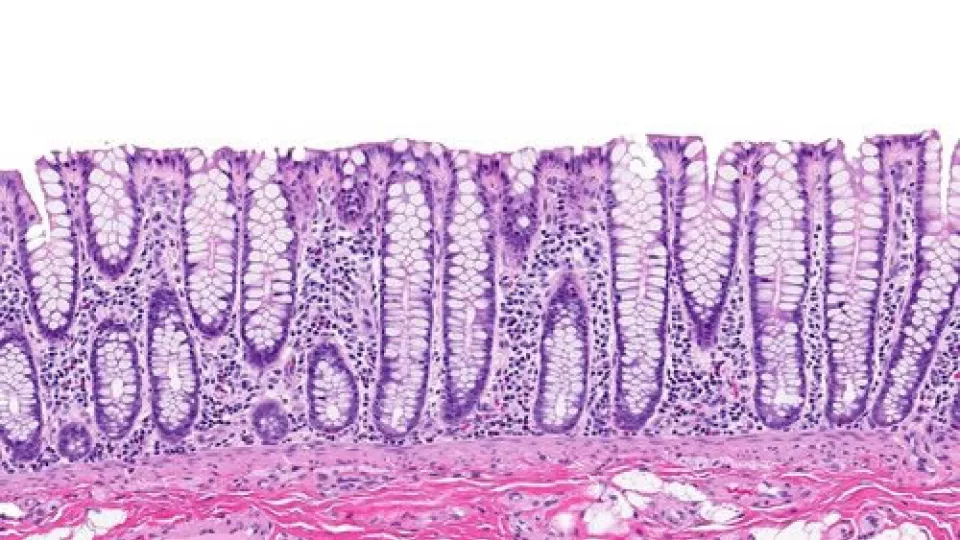
The microbiome is the community of microorganisms—microscopic, living organisms (e.g. bacteria)—that share our body space. In humans, the largest microbiome is in the gut.
What role does the microbiome play in gastrointestinal diseases?
In healthy individuals, the microbiome has many functions and can offer essential nutrients and vitamins. However, disruption in the gut microbiome balance, or “dysbiosis”, has recently been associated with GI diseases such as Crohn’s disease and ulcerative colitis.
Let’s get down and dirty. You’ve completed several fecal transplants in pediatric patients. Is that what it sounds like?
To some degree, yes. A fecal microbial transplant (FMT) is when we introduce the fecal bacteria from a healthy donor into the patient’s colon via a nasogastric tube, colonoscopy or enema.
So how do these transplants help kids with GI disorders?
By sending in healthy replacements, we can return the gut microbiome to its balanced state, which, in turn, can potentially benefit children with GI conditions.
To determine the effect of fecal transplants on specific disorders, we are currently conducting two clinical trials with patients who have recurrent clostridium difficile infection (C. difficile) and ulcerative colitis. Recurrent C. difficile can be very difficult to control, but FMT may offer a new and effective method for preventing future infections. We are also excited about studying FMT in children with ulcerative colitis because current therapies have significant side effects, and some patients may not even respond to those treatments!
Here at CHLA, we have already successfully treated several kids with severe GI disorders via FMT. These patients were unresponsive to traditional treatments, but their symptoms disappeared after the fecal transplant.
What does this mean for the future of gastroenterology treatments and research?
It is our hope that studying FMT will further our understanding of how we can change the gut microbiome of children with GI disorders. This way, we can offer better, and more effective, therapies, resulting in a paradigm shift in how kids with these disorders can be treated.


