That'll Leave a Mark
Long after the aches and pains disappear, our bodies still remember the impact of illness. Barbara Driscoll, PhD, explores how cells use their first experiences with disease to influence future encounters, coining her area of interest “survivor biology.”
“We are imperfect at repair,” says Driscoll, an investigator in the Developmental Biology and Regenerative Medicine Program at The Saban Research Institute of Children’s Hospital Los Angeles. “We survive, but we survive changed.”
These changes generally accumulate over decades. Each bout of flu, pneumonia or bronchitis leaves behind slightly altered cells that impact our overall health and rate of senescence, or the rate at which we age. The process begins during childhood, as some children experience serious stressors earlier than their healthy counterparts. This is especially true in premature infants. Born before their lungs are completely developed, preemies are at risk for such complications as irregular and shallow breathing, respiratory distress syndrome and bronchopulmonary dysplasia.
To study the long-term effects of early health complications, Driscoll utilized a “two-hit” approach in mouse models. The experiment allowed for the controlled observation of elicited respiratory stressors, or hits. Driscoll induced the first hit at 2 months of age—comparable to 25 years in humans—and the second hit seven months later. Now simulating a 40-year-old human organ, the mouse lung was predicted to be fully recovered from the first traumatic incidence. That was far from the truth.
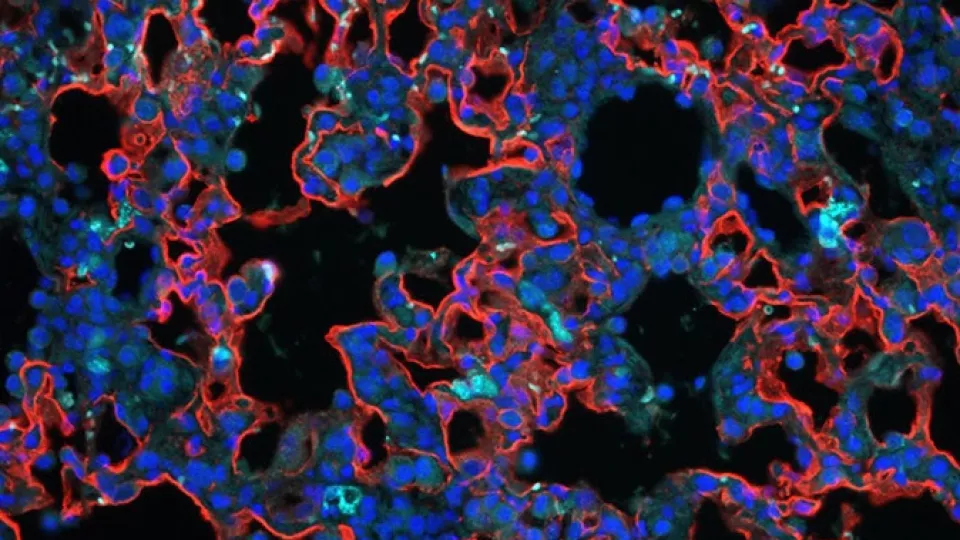
“Scattered, abnormal cell masses, reminiscent of neoplasms, developed in the lungs after the second stressor,” says Driscoll, associate professor of Research at the Keck School of Medicine of the University of Southern California.
One hypothesis for the appearance of these masses suggests that surviving cells retain their memory of past injury. The first traumatic experience may alter mechanisms in the cell cycle, priming an overreaction to future encounters.
“These hits change the organism and the ability of the organism to respond to later hits,” explains Driscoll. “Our goal now is to pinpoint exactly what is altered in these routine pathways and describe the changes as molecular events. Once we do this, we can better respond to these adverse effects and work to prevent them in the future.”
Driscoll is already starting to isolate these changes. Since the regulatory processes disrupted by two hits are the same as those impacted by aging, Driscoll conducted a separate experiment aimed at halting these similarly damaging effects.
She designed a treatment involving an anti-aging drug to be administered to the senescing lungs in a second mouse population. By targeting specific mechanisms in the cell cycle, this therapy slowed down the rate of lung aging and encouraged cell reproduction and vitality.
Driscoll hopes to mimic the condition of pediatric patients by eventually combining both experimental groups. After studying the two-hit approach on lungs that are rapidly aging, she can use the anti-aging treatment to see if it lessens the pathological response observed after a second hit.
“It’s important to remember, especially in young children, that disease doesn’t happen in a vacuum,” says Driscoll. “We always knew that history and context affected disease development and outcome, but we’re just starting to get a handle on how much.”


