Tracking Coronavirus Mutations Shows Early Safety Measures and Travel Restrictions Limited Viral Spread
Scientists at Children’s Hospital Los Angeles used genomic data—information about the virus’s genetic makeup—to examine transmission patterns throughout the United States. Their peer-reviewed epidemiological study, which includes the largest pool of U.S. samples to date, reveals that early rigorous travel restrictions and other measures to control viral transmission limited the spread of this deadly virus. Understanding how the virus behaves and mutates will give research scientists the best chance at developing a useful vaccine. In addition, researchers explain that viral mutation signatures can be used to track patterns in SARS-CoV-2 transmission.
Viral Mutations as Clues for Epidemiologists
When a virus replicates, it makes copies of its genetic material. Mutations—mistakes in the copying process—occur routinely. The errors become embedded in the genome of the virus as it replicates. This means that a particular virus will evolve its own unique signature as it collects these genetic mis-copies. Each new version of the virus, identifiable by its unique combination of genetic mutations, is known as a haplotype.
According to virologists at Children’s Hospital Los Angeles, SARS-CoV-2 mutates about every two weeks. Some mutations may strengthen the virus or make the disease more severe. Other mutations weaken the virus, which may cause that haplotype to die out. The vast majority of mutations are not significant and don’t markedly affect the virus or the disease it causes. Nevertheless, these haplotypes are very useful to scientists.
Each sample of SARS-CoV-2 is like a map of where it has been.
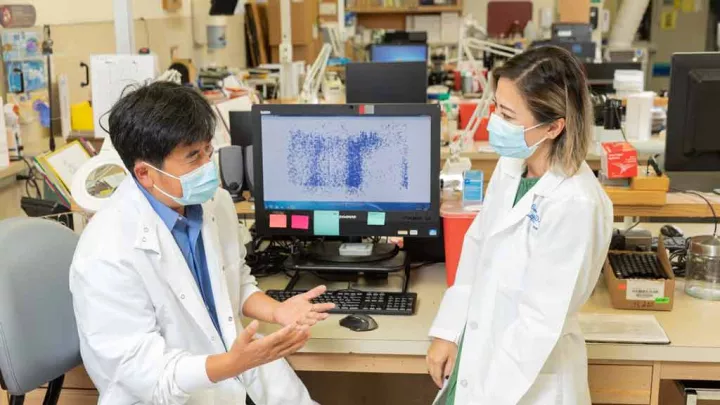
“By looking at the sequences, you can learn a lot about the virus and how it spreads,” says Xiaowu Gai, PhD, Director of Bioinformatics in the Center for Personalized Medicine at CHLA. He explains that while it’s common to refer to the virus, it isn’t really one single entity.
“The virus that infects a patient in California will be different from the virus that infects a patient in Iowa because of how rapidly it mutates,” he says. “If samples from patients this far away from each other don’t differ, we can infer there has been travel between the two states.”
Studying the Genome to Understand Disease Spread
“Fighting a pandemic requires a highly interdisciplinary team of people,” says Dr. Gai. “The world needs clinicians, virologists, pathologists and data scientists. We are so fortunate to have such a team at Children’s Hospital Los Angeles that have worked hard and so well together since the beginning.”
Actually, the team began their work before the beginning, when SARS-CoV-2 hadn’t yet made it to the United States.
Back in February, Jennifer Dien Bard, PhD, could tell a pandemic was imminent. As the Director of the Clinical Microbiology and Virology Laboratory, she recognized the importance of testing and how gathering genomic information can contribute to understanding and battling a disease.
“If we underestimate mutation rate and don’t know how the virus is behaving, any vaccine that is developed could be less effective,” she says. As soon as possible, the team established the SARS-CoV-2 whole genome sequencing assay. “It’s a test that reads out the entire gene library of the virus in each patient sample,” says Dr. Dien Bard. “This gives us a lot of information fast.”
Fast, in a race against a pandemic, is key.
“In those early days of the pandemic, we sprang into action,” says Dr. Gai. “We wanted to develop tools to understand the transmission pattern because it makes a huge impact on how we should be dealing with the virus and the disease.”
After the genomic test was developed, Dr. Gai and Dr. Dien Bard worked with Senior Research Associate Lishuang Shen, testing dozens of samples using their assay. But in order to understand how the virus spreads state to state and globally, the researchers needed many more samples from locations other than California. The team turned to the global scientific community and accessed sequence data from over 6,000 U.S. samples. From this data set, the team was able to identify hundreds of SARS-CoV-2 haplotypes.
Dr. Gai stresses that public data sharing is incredibly beneficial to studies like these. “Institutions all around the globe have been contributing SARS-CoV-2 sequence data,” he says. “The scientific community has done something very important in sharing all of this information.”
Clear patterns emerged from the data. Some haplotypes were found in only one state. These unique, state-specific variants provide evidence that the virus has not spread to neighboring states. Two states – Washington and California – had the highest number of unique haplotypes.
“What we’ve identified with this study is that the states who implemented travel restrictions and safer-at-home orders early during the pandemic were very effective in reducing spread,” says Dr. Gai. “Otherwise, similar mutation signatures would be found everywhere.”
Orders to stay at home, wear masks, and cancel travel have impacted viral spread. “California was one of the few states to implement these measures early on,” says Dr. Dien Bard, “and I think that certainly helped.”
The global COVID-19 pandemic is far from over. But data like these will give the scientific community better tools to understand the virus, which is a critical step in containing it.
“Epidemiological studies can teach us a lot about the virus,” says Dr. Gai. “Moving forward, we will need to continue to follow safety measures because our data show that they work.”