
Non-Alcoholic Fatty Liver Disease: What Physicians Need to Know
Non-alcoholic fatty liver disease (NAFLD) is a spectrum of disease characterized by accumulation of excess fat in the liver (hepatic steatosis) with associated inflammation (hepatitis). While there are many conditions that may cause hepatic steatosis such as hepatitis C, Wilson’s disease (disorder of copper metabolism), and other disorders of lipid metabolism, to name a few, NAFLD refers to hepatic steatosis that is not related to any primary liver pathology and typically associated with obesity. As the prevalence of obesity in children has increased, there is a parallel increase in NAFLD and other obesity-related conditions such as Type 2 diabetes mellitus, hypertension, hyperlipidemia and obstructive sleep apnea (OSA). NAFLD is the most prevalent chronic liver disease in childhood and thus a strong coordination between primary care and pediatric hepatology is essential for timely diagnosis and intervention.
Who should be screened?
Often, patients with NAFLD do not show signs of liver disease in the early stages. The North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN), patients 9-11 years of age who meet these criteria should have a screening alanine aminotransferase (ALT):
- Obese (BMI >95th percentile)
- Overweight children (BMI >85th percentile) with additional risk factors:
- Central adiposity
- Insulin resistance
- Pre-diabetes or diabetes
- Dyslipidemia
- Sleep apnea
- Family history of NAFLD/NASH
- Early screening can be considered in younger patients with risk factors such as:
- Severe obesity
- Family history of NAFLD/NASH
- Hypopituitarism
Age-specific and gender-specific cut offs of the ALT are recommended in interpretation, using 22 U/L for girls and 26 U/L for boys and not referencing the cut offs of the laboratory performing the test. ALT elevation can occur for a variety of reasons, including infection and medications. An abnormal test, considered two times the upper limit of normal, or >45 U/L, greater than three months, warrants evaluation for NAFLD or other causes of chronic hepatitis.
If screening ALT is normal, it is recommended that the ALT be repeated on an annual basis during well-child visits, or sooner if clinical risk factors of NAFLD increase or worsen, such as excessive weight gain or development of other conditions that increase risk of NAFLD, such as Type 2 diabetes or obstructive sleep apnea.
Evaluation of elevated ALT
If screening is positive on two separate occasions three months apart, further work up is warranted. This includes a variety of blood work that screens for conditions known to causes hepatic steatosis listed here with the diagnosis and appropriate work up:
- Infectious etiology
- Hepatitis A – HAV IgG/IgM
- Hepatitis B – HBV surface antigen, HBV surface antibody
- Hepatitis C – HCV Ab
- Autoimmune disorder
- Hypothyroidism – TSH, Free T4
- Celiac disease – serum tTG and total IgA
- Autoimmune hepatitis – antinuclear antibody (ANA), total IgG, smooth muscle antibody (SMA), and liver kidney microsomal antibody (LKM)
- Metabolic disorder
- Wilson’s disease – ceruloplasmin
- Alpha 1 antitrypsin (A1AT) deficiency – A1AT level
- Hereditary hemochromatosis – iron panel (percent saturation, total iron, total iron binding capacity) and ferritin
- Lysosomal acid lipase (LAL) deficiency – LAL activity
We also recommend a screening abdominal ultrasound to evaluate for an anatomic etiology of these abnormalities. Abdominal ultrasound can identify findings consistent with fatty liver disease but cannot distinguish between simple steatosis and steatosis with inflammation/fibrosis (nonalcoholic steatohepatitis [NASH]).
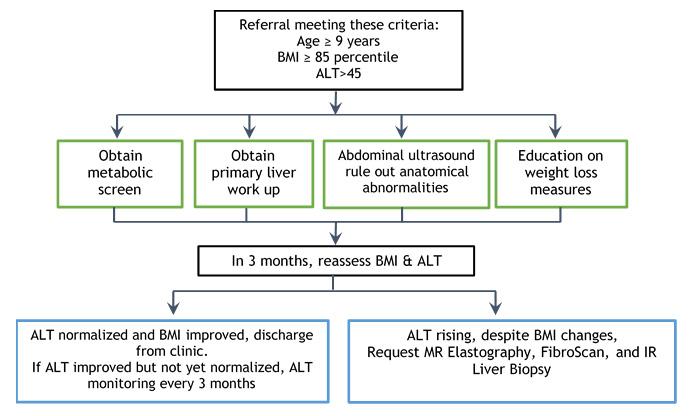
As this work up is being obtained, it is important to refer the patient to the CHLA Fatty Liver Clinic, provided they meet the following criteria:
- Age ≥ 9 years
- BMI ≥ 85th percentile
- ALT >45
In our multidisciplinary clinic, we are able to provide medical, nutritional and psychosocial support for patients referred to us, and determine the need of further interventions and continued management. We screen all patients for diabetes, dyslipidemia, and OSA, and make referrals to endocrinology, cardiology, and pulmonology/sleep study, respectively, as indicated by the screening evaluation.
Children’s Hospital Los Angeles Fatty Liver Disease Clinic algorithm
Diagnosis and treatment of NAFLD
NAFLD is a diagnosis of exclusion and the gold standard for confirmation is a liver biopsy that can be completed on an outpatient basis. The mainstay of treatment of NAFLD/NASH is lifestyle modification. Recommendations that are reviewed include:
- Eliminating all sugar-sweetened beverages (this includes soda, juice, sweet tea, sports drinks, energy drinks and flavored milks)
- Limiting mealtimes per day with snacks
- Appropriate portion sizes
- Appropriate food choices
- Increasing physical activity
If NAFLD/NASH is confirmed, we recommend the addition of vitamin E, 400 IU twice daily. It is not recommended to start this supplement prior to confirmation of the diagnosis of NASH. There are safety concerns that were identified in adult studies, specifically an increased rate of cardiovascular events and prostate cancer in men; however, in the pediatric study, the TONIC trial, no reported adverse events were identified over a 2-year study period. It is recommended that a trial of Vitamin E be initiated for a maximum of two years with the goal of significant response defined as decreased ALT levels.


