How Do You Measure Success in Autism Clinical Trials?
How do you know if a treatment for autism is effective? That’s a question that has no easy answer—due in large part to the heterogeneous nature of autism spectrum disorder.
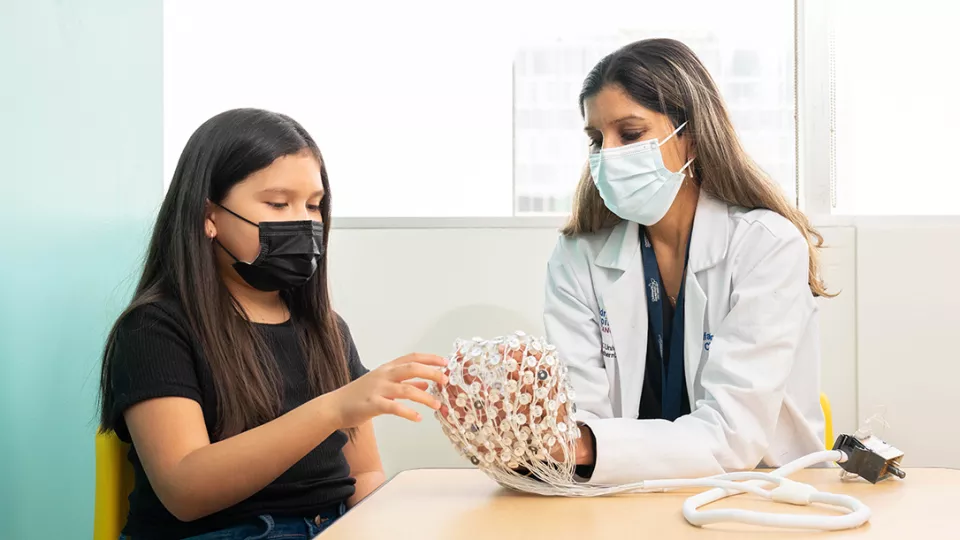
“There’s so much variability in how these children present, what their needs are, what treatments might work, and how they change over time,” says Shafali Spurling Jeste, MD, Chief of Neurology, Co-Director of the Neurological Institute and Las Madrinas Chair at Children’s Hospital Los Angeles. “So how do you know if a drug or treatment is working? It’s not straightforward. We need more objective measures.”
Finding and validating those measures is the goal of the Autism Biomarkers Consortium for Clinical Trials (ABC-CT), one of the largest autism research projects in the country. Children’s Hospital Los Angeles is one of five centers participating in the National Institutes of Health-funded study, which is based at Yale University and also includes Boston Children’s Hospital, Seattle Children’s Hospital and Duke University.
Dr. Jeste is the Principal Investigator for the study at Children’s Hospital Los Angeles and brought the project to CHLA from the University of California, Los Angeles, when she joined the hospital in 2021. She talks about the study, its early findings—and her biggest mission right now.
Why is the ABC-CT so important?
Clinical trials in autism have often struggled. There’s so much variability in the patients, and every study is different in terms of what it’s measuring or how it’s defining change. This variability is particularly problematic in clinical trials, which are studies that are testing whether a treatment could be effective to improve outcomes in children with autism.
The challenge is that we may have a good therapeutic, but we can’t measure its success because we don’t have the right biomarker or patient selection tool, or we may be measuring the wrong endpoints. We need to develop a better infrastructure for clinical trial readiness, and that’s what we’re trying to create by gathering this large-scale data from across the country.
How does the study work?
We’re studying children ages 6 to 11 with autism. They come to our center and undergo a huge battery of clinical assessments. To test biomarkers, we also use electroencephalography (EEG) to measure brain function, eye-tracking technology to measure visual attention, and automated recording techniques to assess behavior and speech.
We then repeat the same tests six weeks later and again at six months. We want to see if these biomarkers and clinical measures are stable or if they change over time, and if they help us identify subgroups within autism. We then compare those same measures in typically developing children. These measures will be used in future clinical trials. Importantly, we give families feedback on these assessments, and parents can use these reports to advocate for services.
What are the early findings?
The team is still analyzing data, but one pretty robust biomarker was in eye-tracking—specifically the time children spent looking at faces. We found that children with autism looked at faces less than typically developing children. This is consistent with what we’ve known from the literature and could be a useful biomarker to follow in treatments that target social attention.
In addition, EEG markers showed that the brain’s response to faces was slower in kids with autism, but we saw quite a bit of overlap with typically developing kids.
The idea is, maybe we could use that biomarker as a way to stratify patients. For example, children who are really slow to process faces might be more likely to respond to a certain treatment, and then we could track face processing as a response to that treatment.
Your team recently authored a paper on medication use in kids with autism. What did you find?
Children who are taking psychotropic medications—for sleep issues, anxiety, behavior issues—are often excluded from autism clinical trials. In this study, we did not exclude children based on medication use, and we found that more than 40% of kids in the ABC-CT study are taking these medicines. Children taking certain medications seemed to have greater overall impairment.
We now can learn about these children and advocate to include them in trials. We need trials to represent those patients we actually take care of in the clinic.
How important is it to include a more diverse patient population?
It’s critical. The demographics of most research studies in autism are overwhelmingly highly resourced white families. At Children’s Hospital Los Angeles, we see an extremely diverse population, including many Hispanic patients and low-income families. Those children have not been in autism studies, for a variety of reasons, such as time, child care, and just the effort needed to engage in these studies. We have to do a better job to make research more accessible to our patients!
There are many potential benefits for families to be in this study. They’re receiving feedback and in-depth evaluations that can help their child, sometimes in cases where they are waiting for months to receive a clinical evaluation. Our goal now is to improve the way we communicate research and make it much easier for all families to participate in autism studies. I want our research to be inclusive and to reflect the amazing patient population that we care for at CHLA. This is my mission!
What’s next for the study?
We are actively enrolling a new cohort of kids to replicate our prior findings, because these biomarkers need to be reproducible. We’ll also be doing a feasibility study for a similar project in children 3 to 6 years old.
I want to make it clear: There will not be one biomarker of autism. But through this work—and through a parallel study going on in Europe—we can optimize our chances for future success in clinical trials. We can learn whether a particular treatment can work, and in which patients. And that will pave the way for new and effective therapies for these children.