Kids with T-cell Leukemia Achieve Remission after Chemo, Even When a Few Cancerous Cells Remain
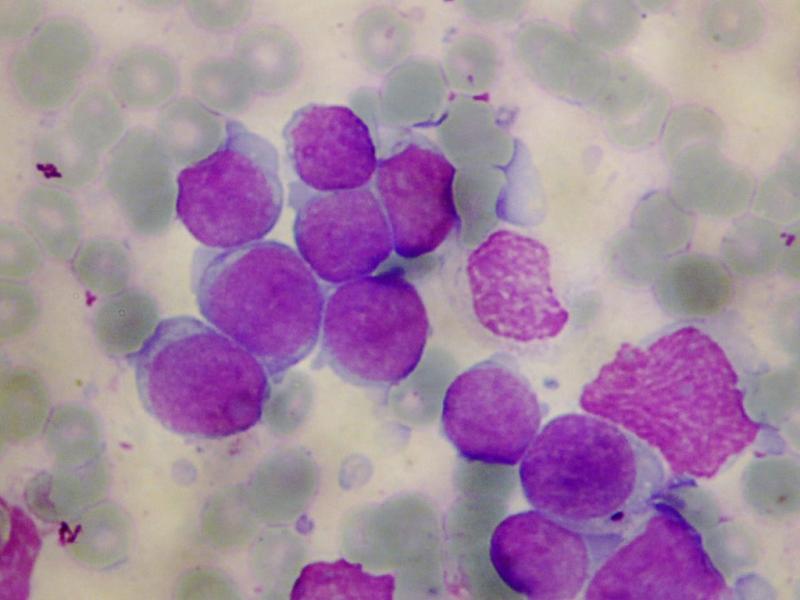
Acute lymphoblastic leukemia (ALL) is the most common pediatric cancer, and includes two subtypes, B-cell and T-cell, depending upon the type of white blood cell where the leukemia originates. For B-cell ALL, the presence of a small number of remaining leukemia cells, called minimal residual disease (MRD), predicts risk of relapse and is therefore used to guide treatment decisions. A team of investigators at Children’s Hospital Los Angeles, led by Hisham Abdel-Azim, MD, conducted a historical cohort analysis and found that MRD alone, at the end of induction therapy, was not predictive of risk or outcome in children with T-ALL. Results of the study were published online in Pediatric Blood & Cancer on May 14, 2015.
“Until now, the dogma has been that for patients with leukemia who have minimal residual disease at the end of induction, we need to intensify their treatment which also increases side effects,” said Abdel-Azim. “We have found for T-ALL, patients have excellent outcomes without therapy intensification and its associated toxicities.”
Following induction therapy, minimal residual disease was determined by flow cytometry for 33 children with newly diagnosed T-ALL and 19 were found to have MRD. At a median of four years follow up, there were no relapses among the patients with MRD and 32 of 33 patients remained in complete remission.
The investigators concluded that clearance of leukemia cells from the blood is slower in patients with T-ALL compared to patients with B-ALL; however, leukemia cells ultimately are cleared without changes in therapy.
Image: T-cell acute lymphoblastic leukemia
Image Credit: Hisham Abdel-Azim, MD, investigator at Children’s Hospital Los Angeles
Additional contributors to the study include Chintan Parekh, MD, and Paul S. Gaynon, MD, both of Children’s Center for Cancer and Blood Diseases, Children’s Hospital Los Angeles and the Keck School of Medicine of USC.
Funding was provided in part by the St. Baldrick’s Foundation, NIH K12HD052954 award, and the Joseph Drown Foundation.