Training Sites
Fellows in the Neonatal-Perinatal Medicine Fellowship at Children’s Hospital Los Angeles train across multiple sites, gaining exposure to quaternary neonatal intensive care, community-based neonatal care, maternal-fetal medicine, neonatal transport, and long-term follow-up. These diverse training environments prepare fellows for a wide range of neonatal conditions, from high-acuity critical care to transitional and outpatient management.

CHLA Newborn and Infant Critical Care Unit (NICCU)
- The NICCU at CHLA is a 58-bed level IV quaternary care neonatal unit. With approx. 550-650 admissions per year, fellows will be exposed to a breadth of high-acuity neonatal patients. Many patients will have multiple pediatric subspecialties and/or pediatric surgery involved in their care. The fellow plays an integral role in coordinating care and collaborating with other services.
- The NICCU serves a wide array of surgical patients. In addition to general pediatric surgical cases (i.e. NEC, intestinal malformations, abdominal wall defects, CDH, pulmonary malformations), many subspecialty surgical patients are cared for at CHLA. Examples include neurosurgery (i.e. neural tube defects (incl. fetal repaired patients), ventricular shunts), ENT and orofacial mandibular team (i.e. tracheostomies, jaw distraction, airway surgery), and a vascular malformation team.
- The NICCU is a regional referral center for neurological evaluation of newborns (including therapeutic hypothermia), as well as genetic and metabolic evaluation. Fellows will gain experience in innovative developmental care such as early detection of cerebral palsy in patients with BPD.
- In addition to general neonatal patient care, the fellows will gain experience in advanced clinical care. Some examples include:
- ECMO
- Renal Replacement Therapies
- Modern ventilatory strategies
- Hemodynamic and neurologic monitoring
- Nutritional strategies for the high-acuity and surgical neonatal patient
- Application of skills acquired in POCUS training in real time patient care.
- Neonatal pain and sedation management, neonatal palliative care, and pediatric bioethics.
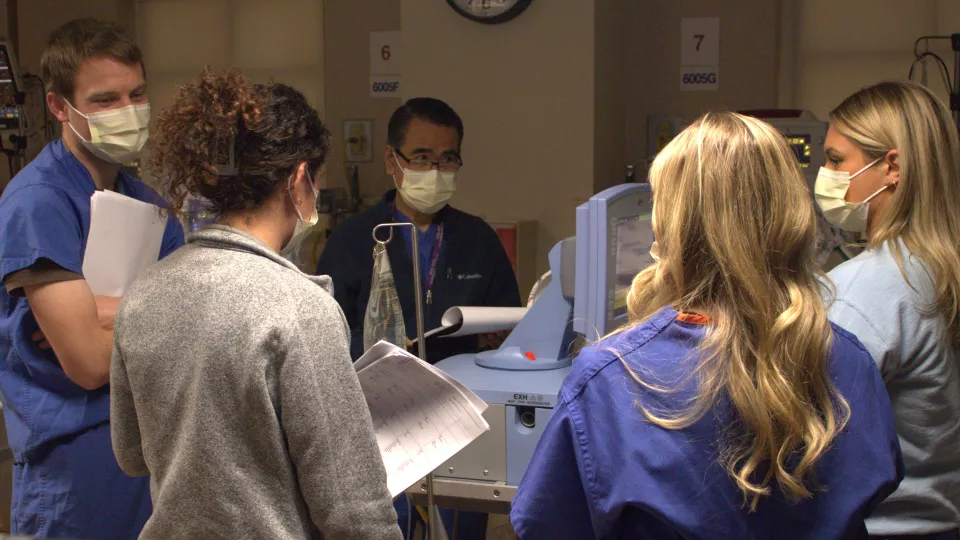
- Patients are grouped in teams according to their underlying problems. We have two general teams, one cardiac disease focused, and a chronic lung disease focused team. The fellows will rotate on all teams over the course of the fellowship, participate in and eventually lead rounds, and take responsibility for patient care under attending supervision.
- Some examples of clinical programs are:
- In the Small Baby Unit, fellows will gain experience with taking care of extremely premature infants who have been referred to CHLA for conditions such as severe lung disease, surgical needs (i.e. NEC, ventricular shunt evaluations, ROP interventions etc.), and PDA management. We offer Piccolo device closure for babies as small as 700g in the cardiac cath lab and even bedside in the NICCU.
- We have one of the busiest neonatal ECMO centers in California which gives ample opportunity for fellows to learn the management of patients requiring this support. The fellows will also gain experience with patients on CRRT (specifically CVVH for ECMO patients and Carpe Diem).
- The CHLA Infant Chronic Lung Disease Program offers opportunity to gain experience in caring for infants with severe chronic lung disease of infancy (CLDi), primarily due to BPD. On the inpatient team, the fellows will gain expertise in modern ventilatory strategies on a daily basis (including decision making for tracheostomy and long-term ventilatory support). Participation on multi-disciplinary rounds with neonatologists, pediatric pulmonologists, pulmonary hypertension specialists, physical/occupational therapists, nurse specialists, dieticians, and respiratory therapists, fellows will learn how collaborate to optimize clinical care and neurodevelopment, how to engage and educate parents, and how to facilitate transition to outpatient BPD care for these complex patients. CHLA is also home to one of the largest home vent programs in Southern California. Patients in the CLDi program are all followed in our multidisciplinary BPD clinic, including those requiring home ventilation. Fellows spend an equivalent of two weeks per year in the CHLA BPD outpatient clinic during their third year to be able to appreciate the trajectory and complexities of long-term care of these patients in the outpatient setting.
- All second- and third-year fellows will rotate for 1-2 months on the Cardiac Cohort team in the CHLA NICCU, which includes caring for a team of 12-14 patients with pre/post-op cardiac disease, arrhythmias, cardiomyopathies, in addition to comorbidities such as prematurity, multiple congenital anomalies, or genetic syndromes. The fellow also provides consultations in the CHLA CTICU, as well as daily rounds with Cardiology Consult team and weekly rounds with the Cardiothoracic Surgeons in addition to weekly teaching rounds with Cardiology/CT Surgery.
- Additional electives in other subspecialties can be arranged based on individual needs and interests.

Hollywood Presbyterian Medical Center (HPMC) NICU
- Located right next door to CHLA, Hollywood Presbyterian Medical Center (HPMC) serves a large population as their community delivery center. The level III NICU at HPMC takes care of neonatal patients with a broad disease spectrum. There are approx. 3300 deliveries per year, and the NICU has 15 licensed beds. We offer many respiratory modalities (including non-invasive ventilation and HFOV), care for ELBWs, and the initiation of whole-body cooling.
- High-risk patients from our Fetal Maternal Institute are commonly delivered here and our team manages those newborns utilizing patient and diagnosis specific delivery plans to optimize the initial stabilization and management. HPMC is also home to the USC fetal surgery program where many interventions (i.e. fetoscopic repair of myelomeningocele, treatment of twin-twin transfusion syndrome, placement of shunts for effusions or bladder outlet obstruction) are performed every month. Being the delivery hospital for many FNI patients, HPMC has one of the highest volume delivery services for newborns affected by fetal anomalies and other life-threatening fetal conditions.
- This diverse patient population offers the fellow a unique training environment where they can get proficient in “bread-and-butter” neonatology and will learn how to resuscitate and stabilize term and ELBW infants alike, as well as infants with congenital anomalies (i.e. congenital heart disease, congenital diaphragmatic hernia, abdominal wall defects, neural tube defects etc.).
Fetal-Maternal Center (FMC) at CHLA
- Located inside HPMC, the Fetal-Maternal Center (FMC) provides unique and comprehensive services to pregnant women who have been diagnosed with a complex fetal condition. The families meet perinatologists and pediatric specialists according to their needs under one roof.
- The FMC sees approximately 1000 patients per year who have a diverse background and with a multitude of prenatal diagnoses. Some examples include congenital heart disease, neurological anomalies, complications of twin pregnancies, genetic conditions, congenital diaphragmatic hernia, abdominal wall defects, intestinal malformations, and many more. Many FMC patients will deliver their babies at HPMC.
- The fellows will spend the equivalent of two weeks as a longitudinal experience at the FMC and the Fetal Cardiac Center. They will have the opportunity to review fetal ultrasound images, fetal echocardiograms, and advanced imaging with attending MFM physicians and Pediatric Cardiologists. Fellows participate in and lead prenatal consultations where they gain skills in formulating delivery plans according to diagnosis and obstetric concerns while taking family wishes into account (including discussions of palliative and comfort care considerations).
Los Angeles Medical Center (LAGMC) NICU
- Los Angeles General Medical Center (LAGMC) is the largest public hospital in the county and one of the biggest public hospitals in the United States. It has been part of the urban Los Angeles community for over 145 years and serves the 10 million residents of Los Angeles County. Los Angeles General Medical Center serves all residents of Los Angeles County regardless of income or background including those who are indigent or receive Medi-Cal only.
- The NICU at LAGMC has 39 licensed beds, about 1,000 deliveries annually, and an average daily census of 17.
- The faculty and hospital staff care for neonates with disease complexity and severity ranging from very high-risk, often extremely premature critically ill neonates born at the Los Angeles General Medical Center to less premature and more stable infants requiring care during the immediate transitional period and beyond.
- In addition, the unit accepts critically ill patients transferred in from different NICUs and the hospital’s emergency room who benefit from the highly specialized and developmentally oriented patient care provided in the NICU at Los Angeles General Medical Center.
- The Los Angeles General NICU also offers specialized neonatal care including treatment of neonatal surgical conditions, Therapeutic Hypothermia Program for neonates with hypoxic-ischemic encephalopathy and a CCS-accredited comprehensive high-risk neonatal follow-up at the Los Angeles General Medical Center.
Maternal Fetal Medicine Rotation at LAGMC
- Fellows will participate in a dedicated two-week Maternal Fetal Medicine rotation at LAGMC where they will learn the evaluation and management of high-risk mothers with pregnancies complicated by such conditions as maternal diabetes, autoimmune disease, pre-eclampsia, as well as fetal surveillance including non-stress testing, biophysical profile, and fetal heart rate monitoring. Fellows will also participate actively in the High-Risk Pregnancy conferences at LAGMC both during this rotation and when rotating through the NICU at LAGMC.
Newborn Follow-Up Program at CHLA
- Fellows will spend 10 half-days per training year in the clinic of the CHLA Newborn Follow-Up Program, supervised by specialists in Developmental-Behavioral Pediatrics. They will have an opportunity to longitudinally follow patients they cared for in the CHLA NICCU and have an opportunity to learn and utilize developmental assessment tools. Fellows will work with a multi-disciplinary team to not only learn the relationship between neonatal illnesses and health and developmental outcomes, but also to become aware of the socioeconomic impact and psychosocial stress that caring for their children places on the family.
Neonatal Transport Medicine

- Fellows will spend two weeks in their 2nd and 3rd year of training at the Access and Transfer (Transport) Center with the transport team while being supervised at all times by an attending Transport Physician. Fellows are required to participate in ground transport of neonates and can volunteer to participate in aero transport.
- The rotation offers exposure to the complete range of pre-hospital care, and transport to and from the hospital by air and ground, from an advanced emergency transport program performing more than 2,200 transports per year. Transport teams are called upon to render expert care to patients with a wide range of pathology, often without the on-site availability of consultants. They must therefore have a broad knowledge base and be comfortable functioning independently yet understand the limitations of their practice. The rotation provides a structured educational transport curriculum for our fellows which assures knowledge foundation and appropriate skill set for neonatal transport. Fellows participate in both didactic and simulation-based training during these rotations.