Michael A. Schumacher, PhD
The focus of our research is to understand the drivers of tissue and cellular remodeling in intestinal inflammatory disease (e.g., ulcerative colitis and Crohn’s disease). Learning how to harness these processes will allow for the development of new tools and techniques to limit chronic inflammation, promote intestinal health, and prevent disease.
Through collaboration with physicians and scientists at The Saban Research Institute, we aim to understand the basic biological processes that shape the intestinal epithelium in response to injury and inflammation. By addressing these fundamental questions, we hope to identify targets that will drive the development of next generation therapeutics for intestinal disease.
Education
2014 PhD, Gastrointestinal physiology; University of Cincinnati
2014 - 2021 Post-doctoral Research Fellow, Gastroenterology, USC, Children’s Hospital Los Angeles
Accomplishments
American Gastroenterological Association
American Physiological Society
Crohn’s and Colitis Foundation
2015-18 Research Fellowship Award, Crohn’s & Colitis Foundation
2018-21 Career Development Award, Crohn's & Colitis Foundation
2021-23 NIH Pediatrics Research LRP
2022 Early Career Author Prize, American Journal of Physiology GI & Liver
Publications
Sprouty2 limits intestinal tuft and goblet cell numbers through GSK3ß-mediated restriction of epithelial IL-33 Nat Commun. 2021 02 05; 12(1):836. . View in PubMed
NRG4-ErbB4 signaling represses proinflammatory macrophage activity Am J Physiol Gastrointest Liver Physiol. 2021 06 01; 320(6):G990-G1001. . View in PubMed
Growth Factors in the Intestinal Tract in Physiology of the Gastrointestinal Tract 2018; 71-101. . View in PubMed
ErbB4 signaling stimulates pro-inflammatory macrophage apoptosis and limits colonic inflammation Cell Death Dis. 2017 02 23; 8(2):e2622. . View in PubMed
Research
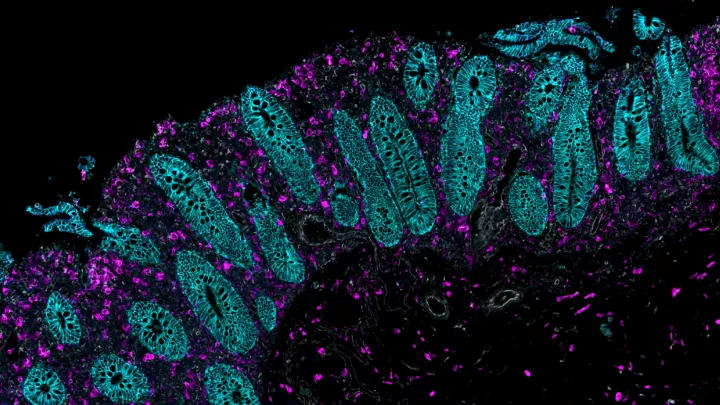
We study the immune and epithelial mechanisms driving tissue remodeling in the gastrointestinal tract. The cellular composition of the intestinal tract is dynamically regulated to appropriately respond to injury, inflammation, and infection. However, the factors driving these tissue changes are not well known. Inadequate responses to insult can result in acute and long-term disease. As these responses are often further impaired by chronic injury and inflammation, as seen in inflammatory bowel disease (IBD), we hope to better understand how to regulate these processes and halt disease.
In particular, we are working to address fundamental questions of how immune signals in the intestinal tract interact with stem and crypt base secretory cells (e.g., deep crypt secretory cells) to promote intestinal health and the response to disease. Despite demonstrations of altered colonic secretory cell numbers in IBD, the mechanisms regulating these cells and their function are poorly understood. We hope to better understand the basic biology and regulatory mechanisms driving these cellular changes in colitis.
Projects in the lab focus on understanding:
- Immune drivers of epithelial cell plasticity during intestinal inflammatory disease
- Regulators of colonic secretory cell function and production of host defense peptides