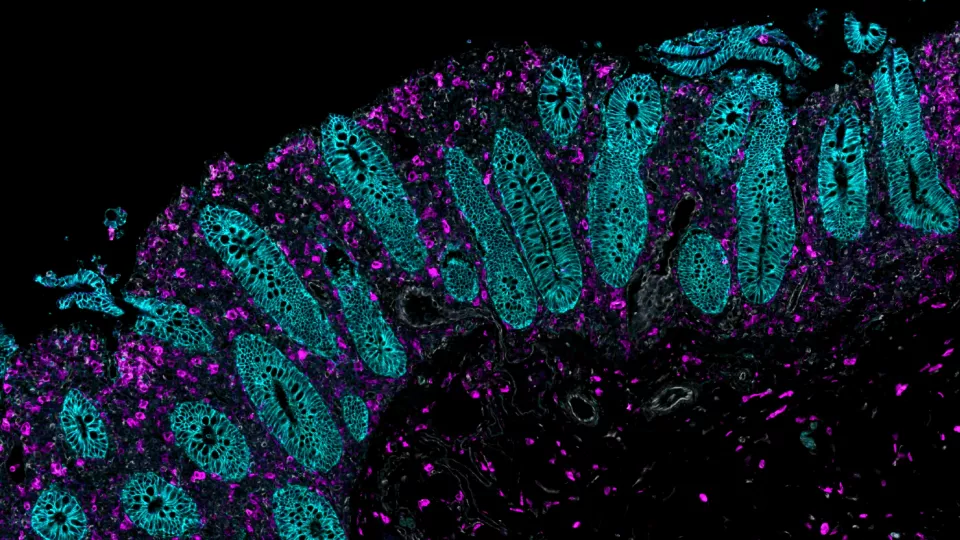
Loss of epithelial lining in colitis. The purple color denotes immune cells that have infiltrated the normal epithelial lining, which is shown in green.
Can a Little-Known Cell Type Lead to New Treatments for IBD?
For decades, the goal of treating inflammatory bowel disease (IBD) has been to control the aggressive inflammation that attacks the colon. Although anti-tumor necrosis factor (TNF) therapies have helped to better manage this inflammation in recent years, up to 70% of patients don’t respond to these drugs long-term.
But what if there was a different way to attack IBD—one that did not involve targeting inflammation? This is the work that Michael Schumacher, PhD, is leading in his lab at Children’s Hospital Los Angeles.

Under a new, $2.7 million grant from the National Institutes of Health, Dr. Schumacher is exploring how to protect the intestinal epithelial lining, which is damaged in IBD. Specifically, he is investigating how deep crypt secretory cells in this lining may promote intestinal healing—and be dysregulated in this disease.
“Our preliminary data suggest that deep crypt secretory cells are hit hard in IBD,” Dr. Schumacher explains. “We want to better understand the basic function of these cells and how they may be contributing to the loss of this critical intestinal barrier.”
A protective role?
Deep crypt secretory cells are one of several cell types in the intestinal lining. Dr. Schumacher’s lab previously found that these cells secrete a protein called RELM-beta, which is known to impact gut bacteria.
Early data from the team also suggests that these cells may be protective of the colon’s stem cell niche, which is critical for the epithelium’s constant regeneration.
“It’s possible that in people with IBD, the regeneration of this lining is impaired because these cells are dysregulated and not secreting the proper ligands,” he says.
Under the grant, the team is using preclinical mouse models to test whether inflammation in the colon is increased—and intestinal repair decreased—when deep crypt secretory cells are impaired. The team is also studying whether amplifying the numbers of these cells will lead to an enhanced healing response.
In addition, researchers are analyzing populations of deep crypt secretory cells to better understand their basic function and to see if certain signaling pathways alter the immune response to gut inflammation.
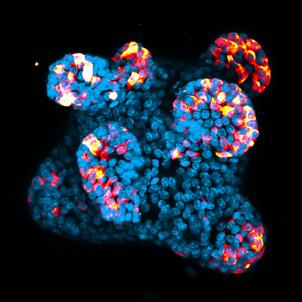
The team is studying many of these questions in organoids—3D structures grown in the lab that mimic the colon. This allows researchers to more clearly see how the epithelium responds to specific factors.
A different way to halt inflammation
Dr. Schumacher adds that his studies benefit greatly from the state-of-the-art research cores at CHLA, particularly the Flow Cytometry Core and Spatial Biology and Genomics Core.
In addition, the team regularly interacts with clinicians at CHLA who provide comprehensive care for children and adolescents with inflammatory bowel disease. Approximately 25% of IBD cases are diagnosed in children under 18.
Dr. Schumacher’s hope is that this research will eventually translate into new treatments and better outcomes for children and adults who don’t respond to current therapies.
“If we can promote the healing of this barrier and maintain its integrity, then we can halt the aggressive inflammatory response,” he says. “The goal is to attack IBD from this different angle and develop more effective treatment options.”


