CHLA Gastroenterologist Provides Guidance on the Use of Intestinal Ultrasound in Inflammatory Bowel Disease Care for New Clinical Practice Update
Mallory Chavannes, MD, MHSc, FRCPC, FAAP, Clinical Director of the Inflammatory Bowel Disease Program at Children’s Hospital Los Angeles, has co-written “AGA Clinical Practice Update on the Role of Intestinal Ultrasound in Inflammatory Bowel Disease: Commentary,” a new clinical practice update from the American Gastroenterological Association (AGA) Institute.
This article, which Dr. Chavannes co-wrote with experts from other institutions and which was published in the journal Clinical Gastroenterology and Hepatology, reviews data and provides guidance surrounding the innovative use of intestinal ultrasound in treating inflammatory bowel disease (IBD).
Faster imaging, speedier decision making

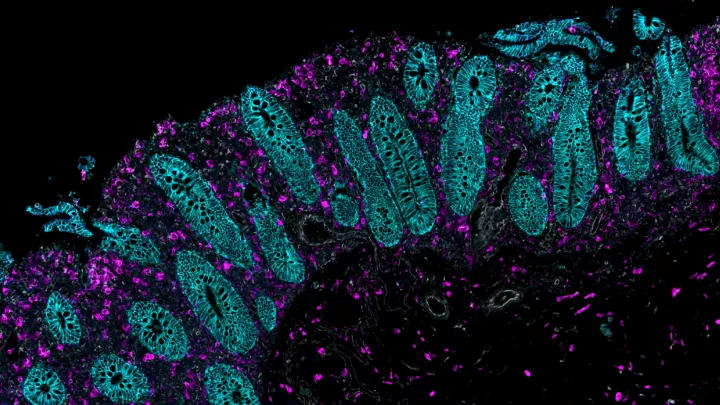
IBD is a chronic disorder that comprises Crohn's disease and ulcerative colitis and is characterized by gastrointestinal inflammation, which without treatment can lead to bowel obstructions or perforation, fistulas and cancer. While the number of IBD treatments are increasing, no treatment works in all patients. Therefore, the cornerstone of managing IBD is monitoring treatment effectiveness at reversing inflammation. Endoscopy is the gold standard monitoring approach, but Dr. Chavannes explains its drawbacks. “Since repeated endoscopies can overburden IBD patients, treatment is often guided through the identification of inflammatory biomarkers. But this requires stool or blood collection, which can be challenging to access or adhere to. Thus, other non-invasive indicators of inflammation are needed.”
Such non-invasive strategies include imaging methods like computed tomography enterography, magnetic resonance enterography, and intestinal ultrasound. Intestinal ultrasound has advantages over these other methods. It does not require oral or intravenous contrast, it is radiation-free, it can be performed in a gastroenterology clinic without a separate radiology appointment, and it is easier to use for child patients.
Dr. Chavannes’ knowledge of these methods comes from her clinical expertise treating patients and from her previous research, which specifically investigated non-invasive IBD monitoring methods. Current research on pediatric intestinal ultrasound and the validation of bowel wall measurement, a marker critical in disease activity assessment, is limited. Dr. Chavannes' most recent original publication challenged the current expert consensus, which extrapolates adult data for pediatric use. With her collaborators, Dr. Chavannes aims to further validate intestinal ultrasound measurements in pediatric patients so that this tool’s routine use becomes more widespread.
One tool with many roles
“Intestinal ultrasound has multiple clinical roles,” Dr. Chavannes says. “It can serve as a screening tool to potentially rule out IBD in certain contexts. It is particularly useful in monitoring IBD patients with comorbidities like obesity or renal failure, who are at increased risk for complications during colonoscopy or other invasive methods. Furthermore, intestinal ultrasound can accurately predict treatment response in real time.”
Intestinal ultrasound does have limitations. It is less precise than magnetic resonance enterography in measuring the length of disease in patients with extensive small bowel Crohn's disease. It is not recommended for dysplasia surveillance—colonoscopy or flex sigmoidoscopy would still be essential. It is also less accurate than endoscopy in assessing disease activity of the rectum and duodenum. In many cases, though, as the new clinical practice update explains, intestinal ultrasound is a practical choice for IBD care.