Childhood Leukemia Isn’t What It Used to Be: Latest Treatments, Research, and Reasons to Hope
Hearing the word “leukemia” can be alarming in any context. Hearing it in the context of your child’s health might feel terrifying, unfair, and even hopeless.
But according to leading pediatric leukemia experts, families grappling with the news of a diagnosis have reason to feel hopeful.
Today, for a great majority of pediatric leukemia cases, a new diagnosis doesn’t mean what it meant 30, 20, or even 10 years ago. Significant advancements in therapies, personalized treatments, and supportive care programs have massively improved the outlook for childhood leukemia, including the most common childhood cancer, acute lymphoblastic leukemia (ALL).
Still, there is no single approach that works for all children with leukemia. When facing ALL, families at Children’s Hospital Los Angeles can access a broad range of treatment options tailored to their child’s unique needs while minimizing side effects.
Seek the experts

The Cancer and Blood Disease Institute at CHLA is the largest pediatric oncology-hematology program in the Western United States. It has been ranked among the top pediatric cancer programs in the country by U.S. News & World Report every year since the rankings were launched in 2008.
The Institute’s doctors are national and international experts in specialty cancer care, having led and developed programs and protocols now used across the globe.
Deepa Bhojwani, MD, leads CHLA’s pioneering Leukemia and Lymphoma Program and has helped uncover several of the field’s critical advances across ALL treatment and research. Here’s what to know about ALL, as well as Dr. Bhojwani’s expert perspective on why families facing a new or potential diagnosis have reason to hope.
What is ALL?
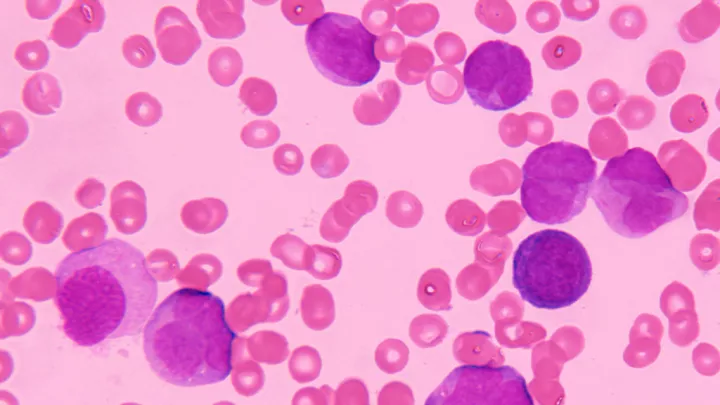
Leukemia is a group of cancers that form in the tissues from which your blood develops.
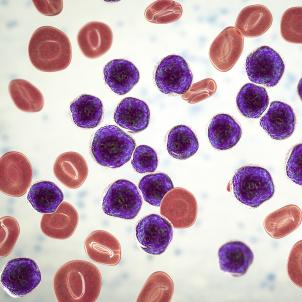
Lymphoblasts are immature white blood cells that are supposed to mature into lymphocytes— “helper” cells that fight disease and infection in the body. Acute lymphoblastic leukemia, also called acute lymphocytic leukemia, is caused by a sudden (“acute”) growth of these lymphoblast cells.
When lymphoblasts replicate out of control without transitioning into healthy lymphocytes, they can cause several problems in the blood, bone marrow, and immune system. This can lead to bone marrow failure, increased susceptibility to infection, and neurological complications.
- B-ALL: The most common type of ALL, accounting for more than 80% of cases in children. In B-ALL, B-cells, the white blood cells that produce antibodies to help fight infection, are affected.
- T-ALL: A less common and more aggressive form of ALL. In T-ALL, T-cells, which directly attack infected or cancerous cells and coordinate the body’s immune response, are affected.
Today, the overall five-year survival rate for children with ALL is approximately 90%.
Genetic testing and diagnosis
“Every child who comes to CHLA with a suspected, new, or recurrent leukemia diagnosis will undergo an extensive workup of their leukemia cells via molecular testing at the Center for Personalized Medicine,” explains Dr. Bhojwani. “We have very, very comprehensive testing that not many institutions have.”
These highly innovative blood tests—some developed by CHLA doctors—can examine and flag abnormalities within the chromosomes, DNA, and RNA of the leukemia cells.
Dr. Bhojwani explains that the newest clinical tests can pinpoint a person’s exact subtype of leukemia, even if it is rare. “As soon as we have that information, we can fine-tune the treatment and give specifically targeted agents for that type of leukemia.”
Treatment options
Chemotherapy: This is the first-line treatment for standard ALL. Chemotherapy uses a combination of medications, delivered by mouth or through an IV or spinal (intrathecal) infusion, to destroy faulty lymphoblast cells, stop overgrowth, and prevent cancerous cells from returning.
Blinatumomab and other immunotherapies: Blinatumomab is a new therapy that uses the body’s own immune cells to target and fight leukemia. Recent studies have shown that blinatumomab can greatly improve outcomes when given with standard chemotherapy.

CAR T-cell therapy: If a patient’s ALL relapses, they may be eligible for a groundbreaking treatment called CAR T-cell therapy. This cell therapy uses genetically re-engineered versions of a patient’s own white blood cells to target and kill cancerous cells. CHLA is home to one of the largest CAR T-cell therapy programs in the country.
Alan S. Wayne, MD, CHLA’s Pediatrician-in-Chief, helped develop CAR T-cell therapy through early clinical trials before the U.S. Food and Drug Administration approved it. “CAR-T therapy has been called the most significant therapeutic advance in childhood leukemia in a generation,” he says of the treatment.
Bone marrow and stem cell transplantation: Bone marrow and stem cell transplants replace the cancer-causing white blood cells with healthy cells from a donor.
For children whose family members aren’t a match for bone marrow donation, there are new, innovative alternatives like haploidentical (half-match) transplants, which CHLA physician-scientists helped pioneer through clinical trials. While these types of transplants generally carry more risk than a full-match transplant, the latest options prioritize safer care and reduced complication risk.
CHLA’s Transplant and Cellular Therapy (TCT) Program has a high survival rate for transplants using stem cells from unrelated donors.
Supportive care
Eliminating cancer is just one part of a comprehensive cancer treatment plan. CHLA’s Survivorship and Supportive Care Program offers proactive services that promote physical and emotional well-being throughout the patient’s entire journey.
“A lot of what we do is help families navigate critical life events—importantly, continuing to grow up,” says the program’s director, David R. Freyer, DO, MS. “You can't put all that on pause while they're in treatment.”

Emotional health: Support services help children learn what to expect and how to cope with the stress of living with cancer. CHLA offers dog therapy, art therapy, and assistance from Child Life specialists, as well as access to social workers and psychologists to help families reclaim peace of mind.
Physical health: Because of the type of cells involved in ALL, cancer can spread to the fluid around the spinal cord and brain and impact function in the central nervous system. When a child is diagnosed, doctors will determine whether their central nervous system has been affected and develop their care plan accordingly.
Additionally, doctors focus on supporting patients’ immune system and organs while they’re undergoing chemotherapy. ALL treatment includes proactive medications to prevent infections, as well as close monitoring of organs like the heart, liver, and kidneys.
Patients might also be prescribed a diet and exercise protocol to ensure the greatest effectiveness of their treatment.
“It’s a very delicate balance of managing side effects while keeping the leukemia away. We have monitoring protocols in place to ensure we don't miss anything,” says Dr. Bhojwani. “We have a whole multidisciplinary team of pediatric cancer specialists at CHLA who collectively manage each patient’s care and modify treatments as needed to ensure their brains and bodies stay healthy.”
Understanding genetic and social factors driving ALL diagnosis and outcomes
Research continues to shed light on how ALL can affect certain racial and ethnic groups in different ways. For example, genetic variants in people of Hispanic ethnicity mean this group is more likely to develop ALL and have higher-risk versions of the disease.
The genetic and social factors that drive these differences are a key focus of continuing research at CHLA. Dr. Bhojwani also highlights the critical need for increased representation of racial and ethnic minorities in clinical, genomic, and biological research: “A more diverse genetic understanding could lead to more effective, personalized treatments.”
Continuing research, from the lab bench to the bedside
A cornerstone of cancer treatment innovation at CHLA is providing families with opportunities to consent to and participate in clinical trials, which are research studies involving people who test the safety and effectiveness of the most promising new therapies and interventions. “Every improvement to pediatric oncology treatment has been made through clinical trials,” says Dr. Bhojwani.
CHLA’s Cancer and Blood Disease Institute is home to the largest clinical trials program in the U.S. for children with cancer and blood diseases.
“We’re focused not only on advancing treatments and making sure they’re available for children around the world but exploring how we can enhance supportive care, improve response to infections, and boost long-term outcomes,” adds Dr. Bhojwani.
Within The Saban Research Institute of CHLA, several labs focus on basic science that can help answer potentially life-changing questions for people with tough-to-treat and relapsed leukemias. “They’re trying to understand why people get leukemia in the first place,” says Dr. Bhojwani, “because we don't yet have the answer.”
“We’re also investigating why some leukemias are more difficult to treat than others,” adds Dr. Bhojwani. “For leukemias that relapse, why, and how does the leukemia cell change during relapse?”
The ultimate goal of these efforts: Bringing access to treatments that cure leukemia quicker—and stop it from coming back.
Ready for anything
Childhood leukemia treatment isn’t what it used to be. Whether you’re facing the prospect of leukemia, a new diagnosis, or a relapse, your care team will ensure your child receives the highest level of treatment, care, and support tailored to their unique needs.
“Though this may be the worst news a parent has to hear—your child has cancer—please know that we are in this together, and there is real hope,” Dr. Bhojwani tells her families. “Leukemia is highly treatable, and children are remarkably strong and resilient. We will be with you every step of the way.”