Recruiting Our Own “Natural Killers” To Fight Cancer
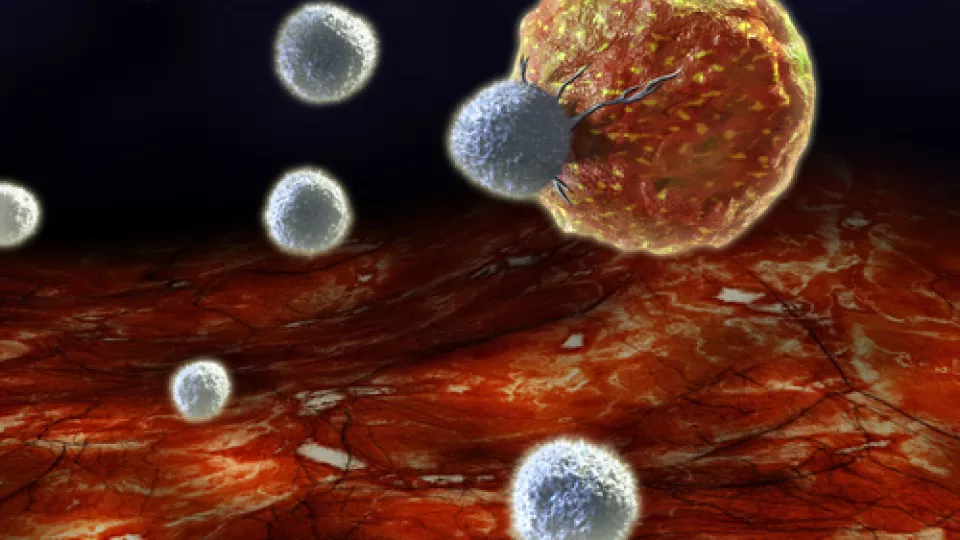
Image: Immune cell attacking cancer cell
There are natural killers in all of us—natural killer cells that is. A critical component of the innate immune system, “NK” cells are specialized white blood cells that are preprogrammed to kill virus-infected cells and tumors. But this ability is hindered in cancer patients, allowing malignant tumors to grow without resistance.
Investigators at Children’s Hospital Los Angeles (CHLA) are helping NK cells recognize, and destroy, their harmful targets in a new approach to cancer treatment. A type of immunotherapy, this technique is one of the ways the body’s own immune system can be harnessed to attack cancer cells. In recognition of the last day of Childhood Cancer Awareness Month, Araz Marachelian, MD, research faculty member of the Cancer and Blood Disease Institute at CHLA, explains the impact of this new therapy:
The main advantage of immunotherapy when compared to traditional treatments is that it works hand-in-hand with the patient’s own immune system to help fight the cancer. The NK cells and other immune cells can be programed to be activated to the right target–the cancer cell. This approach has the potential to better prevent relapses, and it also may be less toxic than traditional chemotherapy and radiation.
There are currently several immunotherapy clinical trials going on here at CHLA. How can this same technique be used to treat different types of cancer?
The reason immunotherapy can be used to treat different kinds of cancers is because our immune system has a major role in interacting with the tumor cells, regardless of the type of tumor. We all have an immune system that we can hopefully learn to harness and work on our behalf to fight cancers. However, for each cancer, variations to the immunotherapy may need to be done to help recruit the right immune cells to do the job.
You are specifically working on immunotherapy in neuroblastoma. What sort of results have you seen so far?
Pediatric neuroblastoma has paved the way for immunotherapy. A recently completed trial showed that, in patients with a very common and most aggressive type of neuroblastoma, giving immunotherapy after completing all other therapy (chemotherapy and radiation) could help prevent relapses and increase long-term survival.
Now, we are working on making that immunotherapy even better by giving it with other drugs (think of them as “helper drugs”) that further recruit the right players of the immune system (the natural killer cells) and work even harder to eliminate the tumor. So far, in our NANT trial, we have seen exciting preliminary data that shows activation of the immune system with the helper drug in patients whose neuroblastoma has recurred. We are hoping to further study this in order to decide whether, in the future, all patients should be receiving this helper medication together with our standard immunotherapy.
What role does immunotherapy play in the future of cancer treatment and research?
Immunotherapy is absolutely the new frontier in cancer research, and it’s a frontier that is changing very rapidly. There are new immunotherapy agents being identified or being engineered to work on the cancer cells, which is very exciting. I think that, for all cancers, it is likely that some form of immunotherapy will become standard therapy in the not so distant future.


