Solving the Mystery of the Silent Stroke
When blood flow is blocked in the brain, a small portion of brain tissue starves and dies – this is known as a stroke. By the time a patient with Sickle Cell Disease (SCD) is 30 years old, he or she has a 50% chance of having a stroke. Children’s Hospital Los Angeles physician and investigator John Wood, Ph.D. is out to discover why. He has dedicated his career to better understanding SCD and improving care for patients with this disease.
SCD occurs when a genetic mutation affects hemoglobin, the component of red blood cells that carries oxygen. This decreases the ability of blood cells to deliver oxygen to tissues throughout the body. It also causes blood cells to deform into a characteristic crescent shape and lodge into the smallest blood vessels, blocking blood flow. This causes excruciating bouts of pain called ‘crises,’ which can severely reduce quality of life. But lurking under the radar is a hidden complication in SCD: the silent stroke.
“We have learned a lot about how to prevent the large vessel strokes,” says Dr. Wood. He is referring to strokes that have immediate, catastrophic effects such as blindness or paralysis. “But patients with SCD still suffer from silent strokes.” Though they are called silent, these strokes can have debilitating effects on the brain’s executive function, which is the ability to execute complex tasks needed for things like maintaining a job or doing well in school. On the surface, the reason for these strokes seems clear: damaged blood cells carry less oxygen, which causes oxygen deprivation in the brain. Yet, Dr. Wood measured total oxygen delivery to the brain and found no decrease in SCD patients. This is because the body compensates for decreased blood oxygen by increasing total blood flow to the brain.
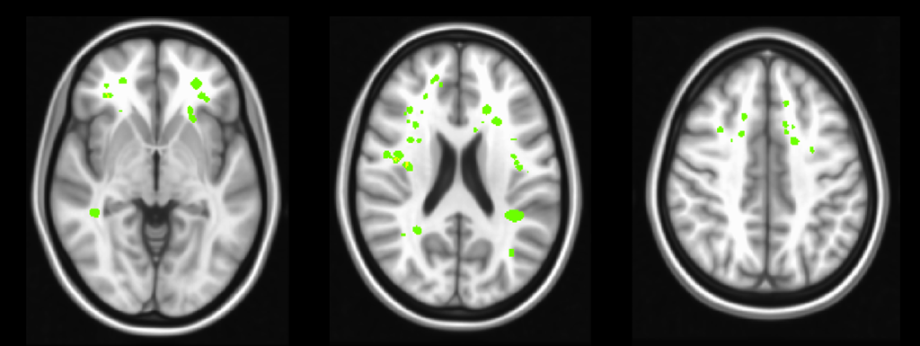
Dr. Wood was left with the question of why patients with SCD continued to suffer strokes. “I began to think, ‘maybe there’s a distribution problem,’” Dr. Wood says. “Total blood flow is fine, but is it going where it needs to go?” Using an advanced imaging technique called arterial spin labeling to measure blood flow, Dr. Wood’s team found a disparity among brain areas. While total oxygen delivery to the brain was unchanged, oxygen delivery to the white matter was reduced by more than a third – 35% – in patients with SCD. Critically, this part of the brain – the white matter – is where the majority of silent strokes occur in these patients.
Grey matter is composed of neurons, the brain cells that store information. White matter is the network of highways in the brain that neurons use to transmit this information. Dr. Wood’s finding demonstrates that the body differentiates between grey and white matter, clearly prioritizing neurons. This makes sense because keeping neurons alive is critical for survival. Strokes in grey matter are immediately debilitating, while strokes in white matter appear silent because they simply cause informational processing to slow. Though they may not cause paralysis or major motor deficits, effects of white matter silent strokes can greatly impede important aspects of a person’s day-to-day life. Dr. Wood’s study gives us a much better understanding of why these strokes are occurring, knowledge that is necessary before medicine can effectively treat this aspect of the disease.
Results of this study were published recently in the American Journal of Hematology by lead author Yaqiong Chai, a senior PhD candidate. The study was funded by the National Heart Lung and Blood Institute of the National Institutes of Health.
Other authors on the study include Adam M Bush, PhD; Julie Coloigner, PhD; Aart J Nederveen, PhD; Benita Tamrazi, MD; Chau Vu, MS; Soyoung Choi; Thomas D Coates, MD; and Natasha Lepore, PhD.
Image caption: silent cerebral infarcts (strokes) are shown in green, overlayed on a structural MRI image. Note that the strokes are found predominantly in the white matter of the brain.