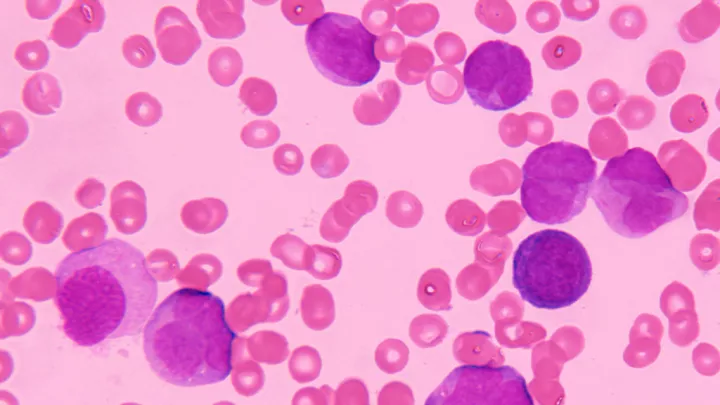
Computer illustration of CAR T-cell immunotherapy
5 Things to Know About Advances in Cancer Research
Experts in the Cancer and Blood Disease Institute at Children’s Hospital Los Angeles are investigating ways to make CAR T-cells more effective—a sort of CAR-T 2.0—as well as genetic and structural approaches for treating various types of cancer.
Here are five things to know about advances in cancer research at Children’s Hospital Los Angeles:

1. CAR T-cells can be made more effective
Chintan Parekh, MD, is studying whether increasing the activity of a T-cell gene called BCL 11B can improve immune recovery after bone marrow transplantation and make CAR T-cells more effective at destroying cancer cells.
“We have generated a roadmap for how T-cells—a type of white blood cell involved in immune response—develop in humans,” says Dr. Parekh. “We are now applying this knowledge in the lab to develop approaches to kick-start immune recovery after bone marrow transplantation and design CAR T-cells against cancer that are more powerful.”

2. CAR T-cells are showing promise against neuroblastoma
It is no exaggeration to say that CAR T-cell therapy has revolutionized leukemia treatment; however, its application in treating other cancers, including neuroblastoma, has been limited due to safety concerns. A group of scientists at Children’s Hospital Los Angeles has developed a modified version of CAR T-cell therapy that shows promise in treating neuroblastoma.
“CAR T-cell therapy is incredibly powerful, but for uses beyond leukemia it has significant barriers,” says Babak Moghimi, MD. “We needed a way to boost the CAR T-cells to make them fight harder and smarter against neuroblastoma. But we also want to avoid injury to brain cells and other healthy tissue.”

3. CAR T-cells are showing activity against solid tumors
Sarah Richman, MD, PhD, is working to find ways to make immunotherapy—including CAR T-cell therapy—an effective, safe treatment for children with solid tumors.
“T-cells have evolved elegant ways to automatically shut themselves down following intense activation in order to prevent autoimmunity,” says Dr. Richman. “However, when we are engineering these cells to fight cancer, those auto shut-off programs may be working against us—especially in solid tumors where CAR T-cells may need an extra boost. We aim to better understand these inherent auto shut-off programs in CAR T-cells in order to engineer them with that extra boost needed to eradicate a solid tumor.”
4. Human stem cell models can be used to identify the underlying causes of pediatric cancers
Miller Huang, PhD, focuses on finding genetic changes that cause healthy cells to become pediatric tumors. Using human stem cell models developed by his lab, Dr. Huang recently identified chromosomal changes as a potential cause of tumor formation in children.
“Unlike in adult cancers, pediatric tumors have few genetic mutations,” says Dr. Huang. “Instead, we believe the cause of pediatric tumors comes from changes in large DNA segments called chromosomes, which mimic the effect of numerous mutations typically found in adult cancers.”

5. The physical properties of cancer cells may offer new treatment opportunities
JinSeok Park, PhD, is applying multidisciplinary approaches to investigate how the “extracellular matrix”—the scaffolding that surrounds cells within tissues—provides the cells with physical support, regulating cancer cell behavior and affecting metastasis of solid tumors such as neuroblastoma and rhabdomyosarcoma.
“My lab aims to understand how this physical interaction between cancer cells and their environment may be cancer promoting—potentially offering therapeutic targets to improve outcomes,” says Dr. Park.