Acute and Chronic Pancreatitis Treatment in Children
Acute pancreatitis in children often requires supportive care, as there is no specific medication to treat the condition. While most children recover within a week, hospitalization can sometimes be necessary to manage symptoms like pain, nausea, and vomiting. Treatment may involve pain management with medication to ease abdominal discomfort, anti-nausea medicine to help your child feel more comfortable, and IV fluids to keep them hydrated. A special diet ranging from clear liquids to regular meals will be recommended once your child is ready to eat again. In rare cases, a feeding tube may be needed to ensure proper nutrition.
Chronic pancreatitis causes permanent damage to the pancreas, loss of pancreatic function, and often requires ongoing care or intervention procedures. Pain management may involve a specialized pain team, and enzyme supplements are often necessary to aid digestion. Dietary changes, such as a low-fat diet and smaller, more frequent meals, are also recommended during an acute attack. If needed, intervention procedures like endoscopic treatments (ERCP) will be performed. In selective severe cases, total pancreatectomy with islet autotransplantation (TPIAT) may be considered to alleviate pain and restore patient’s quality of life. Children’s Hospital Los Angeles was the first to perform this innovative procedure in Southern California and one of only a few nationwide.
Learn more about pancreatitis in children.
Endoscopic Interventions
Minimally invasive endoscopic procedures such as endoscopic ultrasound (EUS) and endoscopic retrograde cholangiopancreatography (ERCP) are often used to treat conditions such as pancreatitis.
Endoscopic Ultrasound (EUS)
This test involves performing endoscopy under sedation or anesthesia with a special flexible endoscope that carries an ultrasound probe. Endoscopic ultrasound helps provide a detailed examination of the pancreas tissue and the pancreatic ducts to identify the stage of pancreatitis. It also has the capability to obtain pancreatic tissue in certain cases to be further examined by a pathologist to identify causes of pancreatitis. Additionally, if there are complications from pancreatitis such as cyst formation or fluid collections, endoscopic ultrasound can be used to drain and treat those fluid collections.
Endoscopic Retrograde Cholangiopancreatography (ERCP)
ERCP is used to look inside the bile and pancreatic ducts. This procedure is done under sedation or general anesthesia and combines the use of an endoscope, a flexible tube with light, and x-ray. The tube is inserted through the mouth down to the beginning of the small intestine. Once there, contrast material is injected into the ducts and an x-ray machine is used to take images. With this procedure, we are able to examine the pancreatic duct, evaluate for strictures and treat them with dilation or stent placement.
Surgery for Pancreatitis
When pancreatitis is chronic or recurrent, and other treatments have failed to relieve symptoms, surgery becomes an option. Children’s Hospital Los Angeles offers comprehensive care to children with pancreatic conditions through our Pancreas Program.
Total Pancreatectomy with Islet Autotransplantation (TPIAT) Surgery
What Is TPIAT?
Children’s Hospital Los Angeles was the first hospital in Southern California to perform total pancreatectomy with islet autotransplantation (TPIAT) for children. Among a few nationwide, we are one of only two centers on the West Coast that offer this innovative procedure. The aim of this procedure is to significantly reduce pain and improve the child’s quality of life.
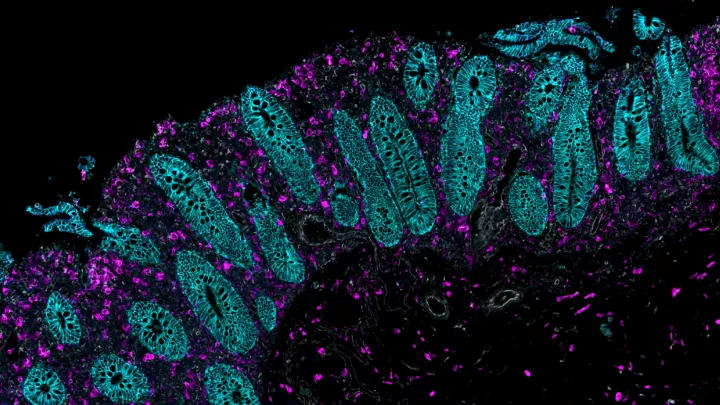
TPIAT involves removing the entire pancreas and reconstructing the gastrointestinal tract. The appendix, gallbladder, and spleen are also removed to prevent complications or due to technical reason. After the pancreas has been removed, it is taken to a laboratory where the hormone-producing cells known as ‘islets’ are isolated and recovered. The islets have beta cells inside them, which are responsible for producing insulin. The islets are returned to the operating room where the surgeon transplants them into your child’s liver where they will continue to produce insulin as they did in the pancreas.
Who Is a Candidate for TPIAT?
Children with acute recurrent or chronic pancreatitis may suffer from debilitating pain, frequent hospitalizations, and loss of pancreatic function. They are unable to attend school or do typical activities and are often hospitalized for their severe symptoms. When all other treatment options have failed, TPIAT might be recommended.
Benefits, Risks, and Potential Complications
One of the main benefits to TPIAT surgery is the pain relief it can provide to the patient leading to an improved quality of life. Within months of recovery, patients can typically return to normal daily activities. Many patients no longer need narcotic pain medication and with time, some will be able to produce enough insulin on their own.
After TPIAT surgery, the patient will be carefully monitored for possible complications. These may include leaks from the biliary or bowel systems, which can lead to infection, bleeding, or blood clots. There may also be elevated blood glucose levels requiring insulin therapy. One common complication is delayed gastric emptying, which can cause nausea and vomiting. This can be managed with medication or a feeding tube. Lastly, there's a possibility that the transplanted islet cells were low to begin with or may not properly engraft, which will be monitored through blood glucose levels in the months after the surgery.
What to Expect Before Surgery
During your child's care at CHLA, you will meet with several specialists during various stages of care who will work closely together on your child’s care plan. TPIAT is a long and complex surgery that lasts most of the day. Here are some things your child will experience before surgery:
- Have an intravenous (IV) line placed and blood tests.
- Continue medications to clean out stool.
- Get an injection to prevent blood clots.
- Be seen by the anesthesia doctor and the surgeon.
- Continue to fast with only clear liquids.
What to Expect During Surgery
There are 5 steps to the operation:
- Your child will be put under anesthesia and closely monitored throughout the operation.
- Both a central line and arterial line will be placed to provide access for frequent labs and medications while your child is in the hospital. The pancreas will be removed, as well as the spleen, appendix, gallbladder, and part of the small intestine (the duodenum). An insulin infusion is started during the operation to control blood glucose levels.
- The pancreas is taken to another facility where the islets will be isolated and recovered. During this time, the surgeon reconstructs the gastrointestinal tract.
- Once the islets are prepared and ready, the surgeon will transplant them through the portal vein, in the liver.
- The surgeon will close the abdomen.
Aftercare and Recovery
Your child will stay in the Pediatric Intensive Care Unit (PICU) at CHLA for close monitoring after their surgery. Recovery times depend on several factors, but most children can expect to be in the hospital for a few weeks. Our care team will manage your child’s pain, monitor blood sugar levels, and check for any signs of infection or other complications. Physical therapists, dietitians, and social workers will assist your child and your family through the recovery process, both during the hospital stay and after your child goes home.
In the months following the surgery, your child will have regular follow-up appointments to monitor their progress. Their blood sugar levels will be closely watched, and in some cases, insulin therapy may still be required if the islet cells do not produce enough insulin.
Distal Pancreatectomy
What is a Distal Pancreatectomy?
Distal pancreatectomy is pancreas surgery where the tail and body of the pancreas are removed. It is used to treat various pancreatic diseases, including pancreatic cancer and severe pancreatitis, although it’s rare in the pediatric population.
Who Is a Candidate for Distal Pancreatectomy?
Children who suffer from severe, chronic pancreatitis or pancreatic cancer.
Benefits and Risks of Distal Pancreatectomy
This surgical option can help remove tumors, cysts or damaged tissue from the pancreas and is considered minimally invasive. The main benefit is relieving symptoms and preventing the spread of disease. However, it can come with risks, such as infection, bleeding, or difficulty managing blood sugar levels. In some cases, your child may need insulin therapy if the remaining pancreas cannot produce enough insulin.
What to Expect During Surgery
Before surgery, your child’s health care team will perform tests to assess their overall health and create a care plan. Your child may need to avoid food and drinks for a certain period before the surgery.
During surgery, the surgeon will remove the tail and body of the pancreas. Other nearby organs, such as the spleen, may also be removed. It is performed under general anesthesia and typically takes several hours.
Aftercare and Recovery
After surgery, your child will stay in the hospital for several days for monitoring and pain management. The recovery time varies, but most children will begin eating and moving around within a few days. Follow-up appointments will help monitor your child’s progress and ensure that the remaining part of the pancreas is functioning properly.
Whipple Procedure (Pancreaticoduodenectomy)
What is the Whipple Procedure?
Also called a pancreaticoduodenectomy, the Whipple procedure is a complex surgery that treats certain conditions by removing the head of the pancreas, part of the small intestine, bile duct, and the gallbladder. The remaining organs are reconnected to maintain normal digestive function.
Who Is a Candidate for a Whipple Procedure?
Those who have been diagnosed with pancreatic cancer or who suffer from chronic pancreatitis might be eligible for this procedure (rarely).
Benefits and Risks of the Whipple Procedure
The Whipple procedure can treat pancreatic tumors, cancers of the bile duct or small intestine, and certain cases of chronic pancreatitis. It can remove cancerous or damaged tissue while preserving the ability to digest food.
Risks include infection, bleeding, and digestive issues. Some patients may have difficulty managing blood sugar levels after the surgery, and in rare cases, complications can include leakage where the organs were reconnected.
What to Expect During Surgery
Your child will meet with our care team to discuss the surgery and undergo tests to ensure they are ready. They will need to avoid eating and drinking for a set period before the procedure, and the anesthesia team will ensure they are comfortable during surgery, which takes several hours. The surgeon will remove the affected parts of the pancreas, small intestine, gallbladder, and bile duct. Afterward, the remaining organs are carefully reconnected to ensure proper digestion.
Aftercare and Recovery
After surgery, your child will stay in the hospital for several days, where they will receive pain management and be monitored closely. The recovery process may take several weeks, and your child will gradually return to eating normal foods as they heal.
Medications for Pancreatitis
Enzyme Supplements
The pancreas normally produces enzymes that help break down food, however, pancreatitis can affect production and make it difficult to digest food properly. These supplements give the body the extra enzymes it needs to begin digestion and reduce the work the pancreas must do which may also help to relieve the pain.
Though enzyme supplements are generally safe, some children may experience side effects like stomach pain, diarrhea, or constipation. Dosage might need to be adjusted to relieve these side effects depending on your child’s reaction.
Vitamin Supplements
A low-fat diet can increase the risk of fat-soluble vitamin deficiencies (A, E, D, and K). Not having enough of these vitamins can increase the risk of severe infections, fractures, cardiovascular disease, and the development of osteoporosis and osteoarthritis. Vitamin supplements are often recommended to help prevent these deficiencies.
Steroid Medications
Steroid medications help reduce inflammation in the pancreas that is caused by autoimmune factors, relieving pain and preventing further damage. They are especially useful when the immune system is attacking the pancreas, as they can help control this reaction and improve your child’s condition.
Long-term use can lead to side effects, such as osteoporosis (weakening of the bones), weight gain, and increased risk of infections. Your doctor will offer guidance on how long your child should take this medication to minimize risks.
Pain Management Medications
Managing severe pain is an important part of treating children with acute and chronic pancreatitis. Pain management includes a variety of approaches:
- Oral Pain Medications: These are often the first step in managing pain and can help reduce discomfort.
- Nerve Blocks: This option targets specific nerves, reducing pain signals from reaching the brain.
- Implantable Pain Pumps: These devices deliver pain medicine directly to the area around the spinal cord, providing long-lasting relief from chronic pain.
It’s essential to work closely with your child’s health care team to adjust their pain management plan as needed.
Pancreatitis Treatment at Children’s Hospital Los Angeles
At CHLA, we offer specialized care for children with both acute and chronic pancreatitis, using a collaborative approach with our experts working closely together. We were the first center in Southern California, and one of the few nationwide, to offer total pancreatectomy with islet autotransplantation (TPIAT) as a treatment option for chronic pancreatitis. We provide expert care customized to your child’s specific needs using breakthrough treatments. Learn more about our Pancreas Program.