Recognizing the Signs of Asthma
Would you know if your child has asthma?

Asthma affects as many as 10 to 12 percent of children in the United States and is one of the leading causes of chronic illness in children. For unknown reasons, the incidence of asthma in children is steadily increasing.
If you suspect your child might have asthma, there’s no need to fear, says Ronald Ferdman, MD, MEd, Chief of Clinical Immunology and Allergy at Children’s Hospital Los Angeles. “With proper treatment and precautions, every child’s asthma can be controlled almost all of the time,” he says.
Dr. Ferdman shares his advice on symptoms, diagnosis, and management and prevention tips for asthma.
What is asthma?
Asthma is characterized by inflammation and narrowing of the bronchial tubes with increased production of sticky secretions inside the tubes, making it hard to breathe.
It's important to note that not all children with asthma exhibit the most obvious symptoms, like wheezing. Chronic coughing may be the only obvious sign, but a child's asthma may go unrecognized if the cough is attributed to other conditions such as recurrent bronchitis or allergies.
While asthma symptoms can begin at any age, most children experience symptoms by age 5.
Symptoms to watch for
Wheezing and/or chest tightness:
Sometimes, children with asthma only experience wheezing or chest tightness with exercise or a cold.
A young child who has frequent wheezing with colds or respiratory infections is more likely to have asthma if:
- Family members have asthma or allergies.
- The child already shows other signs of allergies, including the allergic skin condition eczema or food allergies.
- The child wheezes even when they don't have a cold or other infection.
Frequent cough:
Cough, even without wheezing, is a very common symptom in children with asthma. The cough may be more common at night, and the child may or may not cough up mucus.
While everyone who catches a cold will cough, a common sign of asthma is a cough that lasts much longer than in other people after a routine cold, as long as 2-3 weeks.
Shortness of breath:
Shortness of breath is characterized by a feeling of not getting enough air into the lungs. It may occur only once in a while, or often. Children with asthma commonly note this symptom during any type of physical activity, whether playing formal sports or at recess.
Shortness of breath can also feel like tiredness or a decreased ability to do normal activities. Young children who are not yet verbal may experience feeding problems with shortness of breath while older children may describe tiredness, fatigue, or being unable to keep up with other kids their age.
Diagnosing asthma
Unfortunately, there is no specific test for asthma.
Pulmonary (lung) function tests—often used to confirm a diagnosis of asthma—are difficult to conduct on children under 6 years old. Your doctor may recommend a pulmonary function test to measure how well your child can move air in and out of their lungs. This helps tell your health care provider if your child has lung disease, how severe it is, and which medications may help.
Learn more about pulmonary function testing from the American Thoracic Society.
The diagnosis of asthma in children is usually made by reviewing your child’s symptoms and their response to medications. To help your pediatrician make a correct diagnosis, be prepared with information about your family history of asthma or allergies, your child's overall behavior, breathing patterns, and their responses to possible allergy triggers and medications.
Your doctor may trial several asthma medicines to see if they make a difference in your child's symptoms.
Asthma triggers
An asthma trigger is an activity, condition, or thing that activates asthma symptoms. Recognizing—and, if possible, minimizing your child’s exposure to triggers—is part of a comprehensive treatment plan for asthma.
Common triggers include:
- Weather: Plant pollens and cold and windy weather.
- Household: Dust mites, cockroaches, and pet dander.
- Smoke: Exposure to cigarette or vaping smoke or having contact with someone who smokes (smoke sticks in clothing).
- Chemicals: Household cleaners, citronella candles, bug sprays, colognes, scented lotions, and pool chlorine.
- Stress: Even family stress can contribute to an asthma flare.
- Exercise: Mouth breathing during exercise can exacerbate asthma symptoms. With proper treatment, kids with asthma should be able to participate in sports and physical activity.
Preventing symptoms
There are several ways to help safeguard your child against unnecessary asthma flare ups.
Avoid infection.
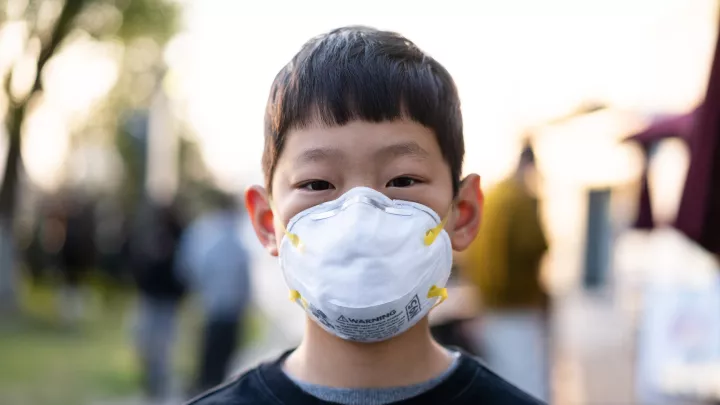
Routine colds and respiratory infections are the most common triggers of asthma attacks in children. Avoiding illness and infection starts with proper hand washing. You should also limit contact with family and friends when they’re sick, stay out of crowds during cold and flu season, and make sure to get your yearly flu vaccine.
Work with your pediatrician.
See your child’s health care provider regularly. Ensure your child takes their medications as prescribed, even when they have no symptoms.
Get an asthma action plan.
Your child's health care provider can help you create an asthma action plan—use it! Make sure your child’s school has a copy of it as well. See an example here provided by the American Lung Association.
Avoid exposure to pollutants.
Alongside household pollutants like second-hand smoke and cleaning chemicals, air pollution can worsen asthma symptoms.
According to the most recent American Lung Association State of the Air report, Los Angeles, Long Beach, and Riverside areas are among the top cities in the nation with the worst air pollution, from ozone to short-term and long-term particle pollution. During wildfires, parents should take extra precautions to minimize their child’s exposure to bad air.
That's why it's so important for local parents to check news reports, air quality alerts from sites like South Coast AQMD and keep children with asthma inside when pollution levels are particularly high.
Pests be gone, and pets beware!
Clean your home regularly and ensure you don’t have pest infestations (such as cockroaches or rodents). Children with severe asthma may also be affected by family pets. Speak with your pediatrician or asthma care provider before making final decisions about having pets in your household.
It may also be helpful to purchase an air purifier with a HEPA filter for your living room and/or your child’s bedroom. Avoid ozone-generating air purifiers.
Don’t smoke.
Cigarette smoke and smoke from vaping can affect your child even if people don’t smoke in their presence or only smoke outside the home.
Don't forget to have fun
Remember—one of the ultimate goals of asthma treatment is for children to remain just as active as their peers while managing their symptoms. Allowing them to play and exercise will help boost their lung function and can even reduce the frequency of asthma attacks.
See more advice from Dr. Ferdman on managing asthma in children.