
The Future of Low-Field MRI for Pediatric Imaging
Recently, John Wood, MD, PhD, Director of Cardiovascular MRI at Children’s Hospital Los Angeles, co-authored a breakthrough research finding: the first real-time, diagnostic quality MRI images of fetal heart disease.
The study, co-led by Dr. Wood and Krishna Nayak, PhD, in the USC Viterbi School of Engineering, takes advantage of a novel technology: low-field, high-resolution MRI. The 0.55 Tesla machine—designated for research purposes at USC—has a magnet that is three to six times lower strength than today’s conventional clinical systems. Children’s Hospital Los Angeles recently purchased its own 0.55T MRI machine as part of its new pediatric cardiac imaging suite, with construction on this suite about to get under way.
For the researchers, fetal cardiac imaging is just the start of their ambitions. The project represents a multicenter collaboration between Children’s Hospital Los Angeles, USC and The Hospital for Sick Children in Toronto.
Dr. Wood talks about the team’s work—and what this technology means for the future of fetal and pediatric imaging.
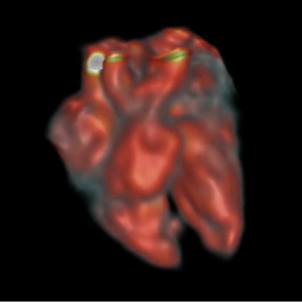
Image credit: JFP van Amerom, et al*
Why are you studying low-field MRI?
There are a number of advantages to using a weaker magnet rather than a stronger one, particularly for any structure in the body that moves or is near air. With a strong magnet, you have a stronger signal—but movement or air can cause distortion in the image. With a weaker magnet, you don’t get that distortion.
This means that lower field strength may be much better for imaging the heart, as well as the lungs and abdomen. And of course, for a fetus, which is always moving! When Dr. Nayak had the vision to develop a low-field program, I was thrilled to work with him. Children’s Hospital Los Angeles is the perfect place to translate this novel idea to pediatric imaging.
What has the team demonstrated so far?
Our most exciting finding has been to perform real-time imaging of a human fetal heart, without the need for cardiac synchronization, using low-field MRI. You can see the fetal heart beating, real-time, which had never been done with MRI.
We’ve also demonstrated that you can do standard fetal MRIs—such as brain MRIs—at 0.55T. When you’re imaging at one-third of the field strength, then the signal is one-third as strong. So we’ve shown how you can make up for that loss of signal.
In June, our team is also presenting additional abstracts at the International Society of Magnetic Resonance in Medicine. Those are demonstrating how you can collect sweeps of these real-time images, re-align them with advanced computer graphic modeling and come out with a much higher resolution picture of the heart.
Why is fetal cardiac MRI needed?
For someone who has good access to medical care, ultrasound often works perfectly. You don’t need MRI. But not everyone has this access, and then it’s sometimes too late in gestation to get a useful ultrasound.
Another issue is body size. A larger body size can make it difficult to get good images from a fetal echocardiogram. When ultrasound can’t diagnose the specific heart issue, you have to wait until the baby is born to figure out what’s wrong. That’s not acceptable. MRI could help fill that gap.

How will low-field MRI benefit pediatric imaging?
Right now, if we do a standard MRI on babies or small children, they need to be under general anesthesia because we need them to stay perfectly still. But if we can use these same low-field tools that we’re developing to image a wiggly fetus to image a wiggly kid—without anesthesia—that’s a big deal.
In the cardiac world, low-field MRI is going to be very helpful whenever there is metal in the body. So right away, even before we’ve developed more advanced acquisition techniques, it could be used for children who have pacemakers or metal cardiovascular devices.
But it’s also going to open up a much broader range of applications, including lung imaging in premature babies or even swallowing studies. The potential is tremendous. Fetal cardiac imaging is the starting point, but our vision is much bigger than that.
What are the next steps?
There’s still a lot of technical development that needs to take place to realize the full potential of this technology. We will be the first pediatric hospital in the world with an FDA-approved high-performance low-field magnet. This is a whole new set of physics we have to master—a lot of programming and post-processing of images. Deep learning and artificial intelligence are going to play a big role in how we produce these images.
That said, when the 0.55T MRI is up and running at Children’s Hospital Los Angeles, I expect it to be a very busy machine from the beginning, even with the techniques we currently have. My hope is that we’ll also be able to translate some of our team’s research advances to the clinical realm. We will be doing a lot of novel imaging on that magnet every day. It’s going to broaden our ability to image a range of conditions in children, and that will give us a tremendous opportunity to advance patient care.
Co-investigators on the project include Ye Tian, PhD, of USC; Joshua van Amerom, PhD, Datta Goolaub, PhD, and Chris Macgowan, PhD, of The Hospital for Sick Children in Toronto; and David Miller, MD, Brendan Grubbs, MD, Jon Detterich, MD, Jay Pruetz, MD, HaiThuy Nguyen, MD, and Skorn Ponrartana, MD, MPH, of Children’s Hospital Los Angeles.
* Fetal cardiac MRI image, full citation: Joshua F P van Amerom, Ye Tian, Datta S Goolaub, John Wood, Jon Detterich, Krishna S Nayak, and Christopher K Macgowan. Fetal cardiac 3D cine MRI at low field - whole heart slice-to-volume reconstruction from real-time spiral SSFP at 0.55T. In Proceedings of the International Society for Magnetic Resonance in Medicine Annual Meeting, Toronto, 2023. p.0548.


