
Team Uses Low-Field MRI to Improve Lung Care for Children

Roberta Kato, MD, has spent the past 10 years working to find an MRI alternative to CT lung imaging in children. Now, a new 0.55 Tesla MRI machine at Children’s Hospital Los Angeles is bringing that dream much closer to reality.
The FDA-approved Siemens FreeMax 0.55 Tesla MRI machine—the first in the nation at a pediatric center—is part of the newly opened Cardiac Imaging Suite at CHLA. But the machine’s potential applications go far beyond heart imaging.
Dr. Kato—a pediatric pulmonologist in Pulmonology and Sleep Medicine at CHLA—is working with John Wood, MD, PhD, Director of Cardiovascular MRI at CHLA, and engineers from the USC Viterbi School of Engineering. She talks about the team’s efforts to harness low-field MRI for children with lung diseases.
Why are you excited about low-field MRI for lung imaging in kids?
What’s most exciting for me is the ability to use low-field MRI to image lung function, not just anatomy. Right now we do lung function testing, which is helpful but does not give a complete picture of lung disease. And it isn’t even possible in babies and young children.
Another advantage is that it will allow us to image the lungs more frequently to better understand and monitor a child’s lung disease. Right now, we can’t use CT scans to regularly monitor or detect lung disease in kids. We want to reduce the potential risk associated with multiple CT scans. Low-field MRI will offer a much better and earlier way to detect lung disease.
Roberta Kato, MDFamilies really want this technology. When I tell them there’s an MRI option, but it’s research, they jump at it.
How are you using low-field MRI to study lung function?
A phase-resolved functional lung scan, or PREFUL, is a new technique that’s used with low-field MRI to spatially quantify lung function—specifically, ventilation and perfusion.
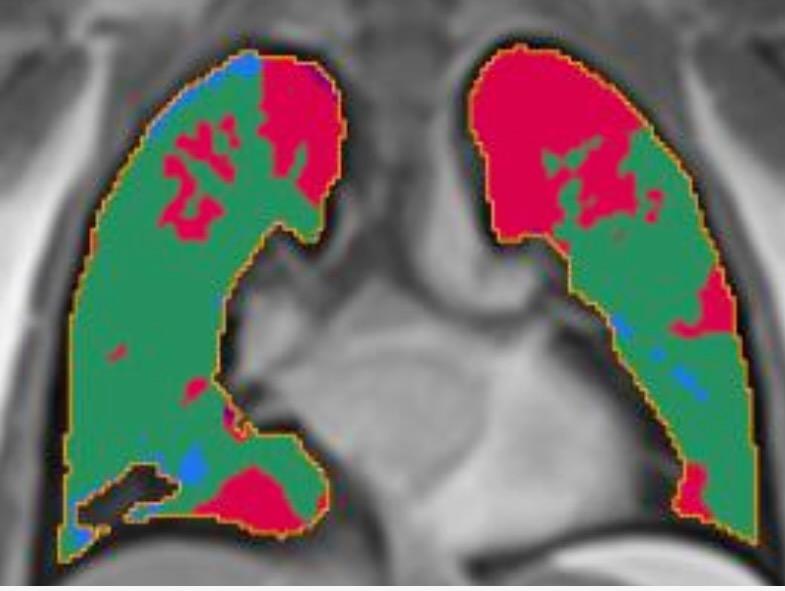
The scan itself only takes five minutes. The data is then uploaded into the PREFUL analysis software, which highlights blood flow and air flow through the lungs. So the red areas indicate perfusion defects, green is normal, and blue shows ventilation defects.
One way we’re using this is to study the lung function of children and young adults with Fontan (single ventricle) circulation. The idea is to understand the precise perfusion and ventilation abnormalities, to see if we can intervene with treatments.
Going forward, it’s also going to allow us to evaluate how patients with cystic fibrosis or asthma or other conditions are responding to therapy. To have objective data on whether a medication is improving lung function is going to be a big step forward in improving care.
What other areas is the team studying?
One of our neonatologists, Narayan Iyer, MD, is using low-field MRI to study the lungs of infants with bronchopulmonary dysplasia (BPD). So we’re using the PREFUL scans to measure ventilation and perfusion, and then we’re also using low-field MRI to look at the lung parenchyma.
The goal is to better understand the baby’s lung disease and optimize how we provide ventilatory support. For babies who have been discharged home, we want to use low-field MRI to monitor how their lungs are developing over time.
What are the current challenges?
The technology is very new. Right now we’re still defining what the normal lung values are for this field strength. Meanwhile, all of this is still research. I think we are still a year or so away from being able to use low-field MRI to make clinical decisions for these patients.
What would you tell other pediatric pulmonologists about low-field MRI?
Families really want this technology. When I talk to parents about a CT scan of their child’s lungs, they hesitate. At CHLA, our CT radiation dose has come down quite a bit, but parents are nervous about radiation. When I tell them there’s now an MRI option, but it’s research, they jump at it.
I would encourage pediatric pulmonologists at other centers to talk to their radiology teams and consider low-field MRI. If they want to be on the leading edge of imaging lung disease in children, low-field MRI—0.55T—is where it’s at. This is the future.


