About the Department of Anesthesiology Critical Care Medicine
The Department of Anesthesiology Critical Care Medicine offers children, families and health care professionals an integrated program of patient care, education and research.
The Department’s role extends outside the operating room setting to include pain management, remote anesthesiology, clinical consultation and critical care services.
Together, our Cardiothoracic Intensive Care and Pediatric Intensive Care units serve more than 2,500 patients annually, while the Comfort & Pain Medicine Program makes 4,000 patient visits each year. Nearly 18,000 anesthetics are performed each year.
Through the Laura P. and Leland K. Whittier Virtual Pediatric Intensive Care Unit, the Department is extending its resources worldwide.
The faculty is comprised of more than 40 members, board-certified in pediatric anesthesiology and critical care medicine. Many of our physicians also are certified in pediatrics.
Clinical Divisions
- Critical Care Medicine
- Cardiothoracic Intensive Care Unit
- Pediatric Intensive Care Unit
- Clinical Anesthesiology
- Pain Medicine
- Palliative Care
Virtual PICU
The Laura P. and Leland K. Whittier Virtual Pediatric Intensive Care Unit (VPICU) connects emergency rooms, community hospitals and intensive care units worldwide in a virtual network – extending telemedicine consultations to even the most remote areas.
By creating a common information space, we are able to benefit critically ill children around the globe. This multifaceted project is funded in large part by the Laura P. and Leland K. Whittier Foundation and the National Institutes of Health.
The vPICU is partnering with other organizations to achieve its vision through the creation of extended databases, education and the extension of access to services via telemedicine networks.
Attendings and Fellows can participate in distance learning through activities posted on the VPICU website and through teleconferencing.
Conference and Resources
Clinical Conference in Pediatric Anesthesiology
Peds CCM
Virtual PICU Website
Department of Anesthesiology Critical Care Medicine Research
The Department has contributed significantly to anesthesia literature over the past several decades, furthering the understanding and growth of this specialty.
Children’s Hospital Los Angeles physician-researchers are actively involved in leading-edge anesthesiology and critical care medicine research. Topics currently being studied include:
- Machine Learning, Data Mining and Artificial Intelligence
- CHLA Respiratory Research Group
- Collaborative Research Networks
- Health Disparities and Equity in Pediatric Pain Management
- Basic Translational Laboratory
- Virtual Reality Analgesia
- Virtual PICU
- Spatial Data Science
Research Areas
Machine Learning, Data Mining and Artificial Intelligence
Randall Wetzel, MB, BS, FCCM, FAAP, has been awarded a Challenge Grant in Health and Science Research by the National Institutes of Health (NIH) National Library of Medicine to research advanced computational frameworks for decision support in critically ill children. The study aims to provide an integrated high-level view of a patient compared to and in the context of previous patients.
Researchers are using advanced computational techniques and artificial intelligence to detect categories in raw medical data from disparate data sources, allowing the most recent information about large numbers of critically ill children to be data mined. This allows researchers to find similarities between a patient and historical populations with known outcomes to enable decision support for diagnosis, management, therapy and outcomes, aiding disease detection, direct patient care, and quality and safety.
CHLA Respiratory Research Group
The CHLA Respiratory Research Group is comprised of investigators from critical care, neonatology, pulmonology, data science, biomedical engineering, respiratory care, nursing, and statistics. The group is led by PIs Robinder G. Khemani MD, MsCI, and Christopher JL Newth MD. ACCM faculty co-investigators include Anoopindar Bhalla, MD, Patrick Ross, MD, and Timothy Deakers, MD, PhD in addition to ACCM staff and lead research respiratory therapist Justin Hotz, RCP. The group is supported by many grants from the National Institutes of Health (RO1, R13, R43/44, K23) as well as numerous foundations and industry sponsors. This group has developed innovative studies related to pediatric mechanical ventilation, respiratory diseases, and pulmonary function.
Ongoing projects include clinical trials and observational studies related to novel modes and methods for mechanical ventilation, measurement of shunt and dead space, patient-ventilator synchrony, advanced monitoring techniques such as electrical impedance tomography, esophageal manometry, respiratory inductance plethysmography, lung and diaphragm ultrasound, ventilator alarms, capnography, respiratory variability, cardio-respiratory coupling, non-invasive estimates of respiratory muscle strength and lung injury, inhalation devices for drug delivery and pharmacodynamics, weaning and extubation. In addition, the group manages a translational lab space to help bring new technologies for respiratory support and management to children, including different ventilator devices, endotracheal tube securement, and non-invasive ventilation. The group provides mentorship to trainees from both CHLA and numerous international institutions.
Collaborative Research Networks
CHLA investigators serve prominent roles in major pediatric critical care research networks. CHLA was successfully funded to be a member of the Collaborative Pediatric Critical Care Research Network (CPCCRN), funded through the National Institutes of Health (RL1) with PI Robinder G. Khemani MD, MsCI and co-investigators Christopher JL Newth MD, Anoopindar Bhalla MD, and John Li MD. CHLA has participated in this network since its inception in 2005 and been integral in the conduct of numerous multi-center clinical trials and observational studies. In addition, several members of the CHLA faculty serve or have served leadership roles in the Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) network (Barry Markovitz MD, Robinder Khemani MD, Anoopindar Bhalla MD), a multi-center network of over 100 pediatric critical care units internationally. CHLA investigators have led numerous studies through both networks.
Health Disparities and Equity in Pediatric Pain Management
Alvina Rosales, PhD is a pediatric psychologist whose research interests are centered on pediatric health disparities and equity. Her expertise lies on psychosocial and cultural factors that impact health behaviors and community-based approaches to improving pediatric health. She was the recipient of a National Institutes of Health (NIH) Diversity Supplement award and has led and collaborated on projects that aim to understand and address Latinx health disparities in pain management. Currently, she is the principal investigator on a mixed-method study examining the use of pain-related social media by youth with chronic pain conditions (funded by the Institute for Nursing and Interprofessional Research). Dr. Rosales is also co-investigator on intervention studies aiming to improve perioperative pain management for underserved youth.
Basic Translational Laboratory
Basic science laboratory equipped to perform translational studies aimed at elucidating mechanisms that contribute to immune dysregulation in disease. We are engaged in collecting and analyzing samples from patients with sepsis, ARDS, and cancer. Current bench-to-bedside research, led by Dr. John Li, involves developing novel immunotherapy treatment strategies for metastatic pulmonary osteosarcoma that encompass testing in preclinical models and translating findings into human cancer.
Virtual Reality Analgesia
For the past 20 years Dr. Jeffrey Gold has been engaged in the implementation and evaluation of virtual reality (VR) focused on patients, their families and healthcare providers targeting health and mental health outcomes (i.e., reducing stress, pain, anxiety, psychological distress), while increasing comfort, satisfaction, and overall positive health outcomes and wellness in children/adolescents undergoing routine painful medical procedures. Dr. Gold has been identified as a pioneer in the world of pediatric VR contributing early to the scientific literature long before VR was commercialized. Early studies focused on routine blood draw and IV placement, while recent studies have focused on sedation sparing VR procedures, such as the use of VR for transnasal endoscopy, MRI preparation, and VR for mask induction. Dr. Gold is involved in numerous VR clinical trials examining the impact of VR for pain management. Dr. Gold is also involved in international efforts to elevate, discover, educate, and investigate the application of VR for chronic pain management. Dr. Gold is a recognized international expert in pediatric VR and collaborates world-wide, including being a member of the Interdisciplinary Network on Virtual and Augmented (AR/VR) Technologies for Pain (INOVATE-Pain).
Virtual PICU
Every day doctors observe the outcomes of the treatment they provide for thousands of patients. These experiences serve as practical therapeutic trials, conducted on a patient-by-patient basis. With the increasing adoption of electronic health care records, hospitals and clinics are collecting data from thousands of these experiments daily. However, much of it remains inaccessible and unsearchable, and providers are unable to learn from this vast accumulated experience. The Laura P. and Leland K. Whittier Virtual Pediatric Intensive Care Unit (VPICU), led by Dr. Randall Wetzel, aims to create a common information space for the international community of caregivers providing critical care for children. The VPICU will build extended databases to allow inter-institutional data sharing to create extended, multi-center knowledge bases. The VPICU will also improve education, quality enhancement and telemedicine in this field.
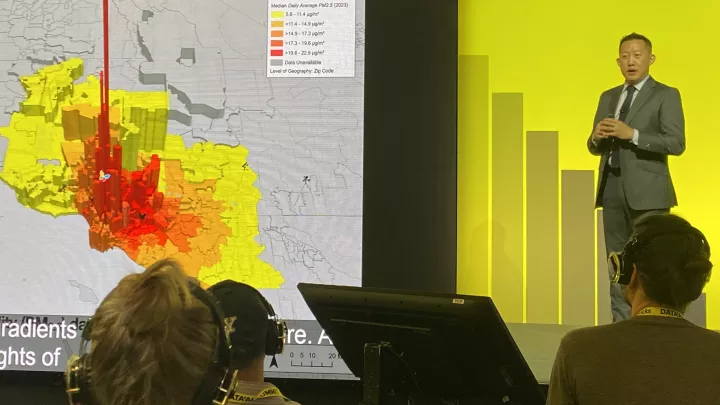
Spatial Data Science
Dr. Jonathan Tan focuses on developing spatial data science methods to understand the impact of where a patient lives and social determinant of health risk factors on pediatric patient safety and health outcomes. He has been awarded grant funding from the Anesthesia Patient Safety Foundation (APSF) and Foundation for Anesthesia Education and Research (FAER) to study the environmental risk factors that pediatric patients may have when undergoing anesthesia for surgical procedures. The grant proposes a single-center prospective cohort study that will examine spatiotemporal effects of indoor and outdoor air pollution exposure (PM2.5, PM10, and NO2) and neighborhood- level socioeconomic risk factors that are associated with Perioperative respiratory adverse events (PRAE) in children undergoing general anesthesia for elective ENT procedures.